It has recently become apparent that patients with COPD commonly suffer skeletal muscle dysfunction, which may be the main cause in the reduction in exercise tolerance.
COPD patients tend to reduce their levels of physical activity as it causes unpleasant effects and results in a vicious cycle where a reduction in physical fitness leads to further impairment of muscle function
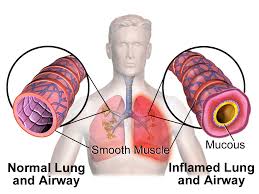
Skeletal muscle dysfunction is very common in patients with COPD, and may play an important role in limiting exercise performance. Muscle strength and endurance are both decreased and the muscle is more easily fatigued. Muscle atrophy is largely responsible for the reduction in muscle strength but deconditioning is of major importance as well as nutritional depletion, and steroid use. COPD may also produce a systemic inflammatory response that may adversely affect skeletal muscle function.
Muscle strength is seen to be decreased in patients with COPD and particularly in the lower limbs. An important factor is muscle wastage; either through medical reasons or a lack of exercise due to breathlessness. Muscle endurance and the length of time the muscles can be used also decreases significantly. In biopsies the ratio of different muscle fiber types are altered in COPD patients and type IIa convert to type IIb, resulting in reduced muscle endurance, increased fatigue and a reduction in muscle mass. The number of capillaries within the muscle is also significantly lower in COPD patients as well as the number of mitochondria. Enzymes that are required for metabolism within the muscles are also decreased in COPD patients. This all results in less oxygen reaching the muscle cells and metabolism and function of the cells being adversely affected.
Medications such as steroids which are used to treat exacerbations can also cause muscle wastage. Short-course doses are beneficial to the patient but long-term multiple short-courses requires further study.
Malnutrition is also common with COPD where 35% are less than 90% of their ideal body weight. This results in a reduction in muscle mass and metabolic functions are disrupted. Nutritional supplements however are not a substitute for eating a balanced, healthy and high in calories food plan. Patients can tend to either put on weight from a lack of mobility or lose weight from the increased energy required to breath and a reduction in appetite due to the difficulty of eating and breathing with breathlessness and the need for constant oxygen supplementation.
Deconditioning from disuse is believed to be the major contributing factor in the skeletal muscle dysfunction observed in patients with COPD. When healthy individuals undergo a training program to increase fitness levels physiological and morphological changes are seen and results in muscle larger in mass with increased oxidative capacity and more efficient in its ability. From previous studies it was thought that COPD patients could not reach the same levels of increased muscle efficiency when undergoing the same training program. However studies have shown that a certain level of intensity and duration needs to be reached before the muscle will begin to improve.
Exercise training will improve skeletal muscle function in those with COPD and pulmonary rehabilitation is shown to improve endurance capacity and quality of life, however the type of exercise training should be further studied and bespoke personal exercise plans developed for individuals to to get the maximum potential from their exercise.
Oxygen therapy is provided for patients to help them to breathe but long-term oxygen therapy has been shown to help improve muscle function and metabolism. It also reduces the potential harm of deconditioning as patients on oxygen therapy tend to be more mobile and physically active as they benefit from the positive benefits of supplemental oxygen.
Muscles require constant use, a balanced supply of metabolites from our diet and oxygen in order to work efficiently. Studies have shown that oxygen therapy not only directly affects muscle function positively but it enables patients to be more physically active and exercise more frequently and for longer, which in turn reduces potential deconditioning and helps to build up muscle mass, strength and efficiency.
REFERENCES: www.ncbi.nlm.nih.gov and www.respiratory-research.com