How Do Different Devices Provide My Oxygen?
Oxygen therapy is administered in a variety of ways depending upon the circumstance, the patient's requirements and the devices used. It is required in order to provide additional oxygen to the patient and to increase the level of oxygen in the body needed by your body to function.
In most cases the oxygen first passes through a pressure regulator which controls the oxygen pressure as it passes from an oxygen cylinder to the device which is at a lower pressure. Once the oxygen is at this lower pressure, the flow of the oxygen can be controlled by a flow-meter and is measured in litres of oxygen per minute (lpm). The usual flow rate for most devices is between 0 and 15 lpm but can be as high as 25 lpm in some units. Many flow-meters are based on a 'Thorpe tube' design which can be set to 'flush' which is useful in an emergency situation.
In room air the content of oxygen is only 21%, which although is adequate for healthy individuals, needs to be increased to help those with certain diseases or medical conditions in order to increase the oxygen that manages to get through to their blood stream. Usually increasing the oxygen to 30-35% is enough to make a significant difference and this can be achieved using a nasal cannula, a thin tube with an individual tube for each nostril. This can provide the oxygen at a low flow rate (0.25 to 6 lpm) to achieve an oxygen level of 24-40%.
To achieve higher oxygen concentrations various face masks can be used including a simple face mask, which can deliver oxygen at 5-15 lpm to achieve 28-50% oxygen levels. The Venturi mask can provide oxygen up to 40% and a partial re-breathing mask, which includes a reservoir bag attached to it can provide oxygen at between 40% and 70% concentration.
For patients requiring 100% oxygen the most common device is the non-breather or reservoir mask. This is similar to the re-breathing mask but has a number of valves to stop air that has been exhaled from the lungs from returning to the bag. At a flow rate of 10 lpm up to 80% oxygen levels can be achieved.
For patients requiring the therapy on a constant long-term basis, the oxygen can be warmed and humidified before administration through the nasal cannula to prevent irritation and dryness.
If a patient cannot breathe independently then positive pressure may be needed to force air into the lungs, which is provided by complex artificial respirator machines such as ventilators or a continuous positive airway pressure machine.
References: http://www.news-medical.net and http://www.nhs.uk/conditions/home-oxygen
Travelling with Oxygen: How Does My Oxygen Concentrator Work?
Over the years, portable oxygen technology has developed and combine with travel really assists in maintaining those who require supplemental oxygen the ability to travel across the globe. This article explores these developments, the safety aspects and tips for oxygen assisted travel today.
Understanding Portable Oxygen Concentrators or (POCs)
Portable Oxygen Concentrators mean that you can have your oxygen therapy as you move. These compact devices:
1. Extract oxygen from ambient air
2. Deliver purified oxygen to the user
3. Operate on rechargeable batteries
4. Are approved for use on most airlines
How POCs Work
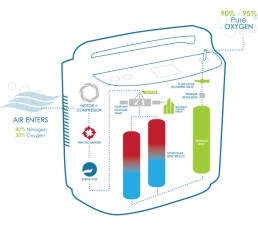
POCs utilise 'pressure swing adsorption' technology:
1. Compress ambient air
2. Remove nitrogen using zeolite minerals
3. Concentrate oxygen to 90-95% purity
4. Deliver oxygen via pulse or continuous flow
Latest POC Innovations
- Lighter weights (some under 5 lbs)
- Extended battery life (up to 8 hours)
- Smart device connectivity for monitoring
- Quiet operation for discreet use
Travel Planning with Oxygen
1. Consult Your Doctor
- Obtain travel clearance
- Discuss oxygen needs at different altitudes
2. Contact Airlines in Advance
- Confirm POC approval
- Arrange for in-flight power sources if needed
3. Pack Essential Supplies
- Extra batteries
- Power adapters for various outlets
- Nasal cannulas and tubing
4. Research Destination Healthcare
- Locate oxygen suppliers at your destination
- Know emergency medical facilities
5. Consider Travel Insurance
- Ensure coverage for oxygen-related needs
Safety Tips for Oxygen Travel
- Keep POC in carry-on luggage
- Bring prescription and doctor's statement
- Avoid smoking areas and open flames
- Stay hydrated, especially during air travel
Choosing the Right POC for Travel
Factors to consider:
- Flow rate requirements
- Battery life
- Weight and size
- Noise level
- FAA approval status
Overcoming Travel Challenges
- High-altitude destinations: Consult your doctor about adjusting oxygen flow
- Extended trips: Research oxygen refill options at your destination
- International travel: Check voltage compatibility and plug adapters
The Future of Oxygen Travel
Emerging technologies promise even more freedom:
- Wearable oxygen devices
- Improved battery technology
- Integration with smart health monitoring systems
With proper planning and the right equipment, oxygen therapy users can explore the world with confidence.
The Difference Between Pulse And Continuous Flow
At OxygenWorldwide, we understand that oxygen therapy shouldn't limit your wanderlust. Let's explore how portable oxygen concentrators (POCs) are revolutionizing travel for those who need supplemental oxygen.
The Evolution of Portable Oxygen
Since 2000, POCs have transformed from bulky machines to sleek, travel-friendly devices. They offer two main types of oxygen delivery:
1. Continuous Flow: Ideal for patients with high oxygen needs
2. Pulse Flow (On-Demand): Perfect for more active users
Continuous Flow POCs: Steady Support
• Provide uninterrupted oxygen supply
• Preferred by patients with severe respiratory issues
• Offer mobility, but may use oxygen faster
Pulse Flow POCs: Efficiency Meets Portability
• Deliver oxygen only when you inhale
• Conserve oxygen, extending usage time
• Lightweight (around 2kg) and highly portable
• Suitable for high-altitude travel
Dual-Flow POCs: The Best of Both Worlds
• Combine pulse and continuous flow options
• Cater to a wider range of oxygen needs
• Slightly heavier (5-10kg) but often come with wheels
Choosing Your Perfect Travel Companion
When selecting a POC for your adventures, consider:
1. Your prescribed oxygen flow rate
2. Battery life and charging options
3. Weight and portability
4. Altitude performance
5. Noise levels
Sleep Considerations
• Pulse-flow POCs may not be ideal for all sleep situations
• Some modern POCs adjust to slower nighttime breathing
• Continuous-flow mode is often preferred for CPAP users
OxygenWorldwide's Travel Tips
1. Consult your doctor about your travel plans
2. Familiarize yourself with your POC's features
3. Carry extra batteries and charging accessories
4. Know your oxygen needs at different altitudes
5. Check airline policies before booking
The Future of Oxygen Travel
At OxygenWorldwide, we're excited about emerging technologies that promise even greater freedom:
• Smarter, more responsive POCs
• Longer-lasting batteries
• Integration with health monitoring apps
Conclusion
Don't let oxygen needs ground your travel dreams. With the right POC and proper planning, the world is yours to explore. OxygenWorldwide is here to support your journey every step of the way.
Misdiagnosis of COPD is Common and Dangerous
There are many stories of patients being misdiagnosed and given treatment for asthma when in fact years later the patient is then diagnosed with COPD.
Pat Crowe was a healthy, active 39 year old but was told he had developed asthma and was given an inhaler. Over the next few years his health deteriorated, he grew dependent upon and overused his inhaler, suffered from side effects and eventually the inhaler wasn't enough. Being so breathless meant his confidence plummeted, making him almost housebound.
'I panicked about going outside and crossing busy roads because I was having trouble breathing and couldn't move quickly.'
During bad spells and prolonged attacks he was also prescribed strong steroid pills, which caused side-effects, including a swollen face and hunger.
'My wife became my carer, and my family were very scared watching me struggle to breathe,' he says. 'I didn't even want to get out of bed and go down stairs because I was worried about getting back up. My life changed completely.'
It was only then that Pat's consultant performed a spirometer test which confirmed that he didn't have asthma after all but suffered from COPD, which explained why he'd found the condition impossible to control.
COPD is incurable and affects 900,000 people in the UK, usually above the age of 35, and an estimated 30,000 people die from it each year. Experts believe there are also more than two million undiagnosed cases.
Specialist advice is crucial when it comes to achieving an accurate diagnosis says Dr Kurukulaaratchy: 'GPs need better awareness of these conditions. They both rank highly in hospital admissions, but if management is right early on, you can improve quality of life and possibly even life expectancy.'
Nick Hopkinson, honorary chest physician at the Royal Brompton Hospital, London, adds: 'Asthma patients usually have normal lung function, but when they experience asthma symptoms or an attack their airways go into spasm, becoming narrow and inflamed. Then, after taking medication - usually an inhaler - their lungs return to normal. However, COPD patients have relatively fixed lung disease, so even on a good day they still have symptoms. Most of the damage isn't reversible and progressively worsens.'
One major consequence of misdiagnosis is that patients could be given the wrong medication.
COPD patients usually start with bronchodilator inhalers to relieve narrowing of the airways and then go through a variety of drugs, starting with shorter-acting medications and moving to longer-acting ones, as the disease worsens, says Dr Kurukulaaratchy.
'Research has shown steroids can lead to an increased risk of pneumonia (inflammation of lung tissue) in COPD patients, so this is a risk if they are wrongly labelled as having asthma.'
If the condition doesn't improve, they can end up using a lot of steroids, which have side-effects such as weight gain, mood changes and osteoporosis.
'If patients are told they have COPD but it's asthma and they don't have inhaled steroids, they won't be able to control the disease - leaving them prone to worsening symptoms and even death from an asthma attack,' says Dr Hopkinson. 'We see 1,100 asthma deaths a year in the UK, often because they weren't on preventer treatments.'
Also oxygen therapy treatment is a major component of COPD treatment which is prescribed by your doctor, so if you are misdiagnosed then you may not be prescribed oxygen as early as you should have been which can affect your health and long-term diagnosis as COPD damage to the lungs is irreversible.
If you have any doubts about your diagnosis then speak to your doctor or get a second opinion, just to be sure as your health is the most important thing.
References: http://www.dailymail.co.uk
Lifestyle Tips To Manage Your COPD
Living with chronic obstructive pulmonary disease (COPD) doesn’t mean you have to stop living your life. Being on the correct medication and oxygen treatment regime is crucial but there are some tips on lifestyle changes that you can make to help you manage the disease.
Stop Smoking
Smoking is the number one cause of chronic bronchitis and emphysema. Together these diseases comprise COPD. If you haven’t already quit, it’s very important to take steps to stop smoking. Talk to your doctor about smoking cessation strategies.
If nicotine withdrawal is a concern, your doctor may be able to prescribe nicotine replacement therapy to help you slowly wean yourself off. Products include gum, inhalers, and patches.
People with COPD should avoid all inhaled irritants such as air pollution, dust, or smoke from wood-burning fireplaces.
Defend Against Infections
People with COPD are at risk for respiratory infections, which can trigger flare-ups. Infections that affect the airways can often be avoided with good hand-washing hygiene. Cold viruses, for instance, are often passed through touch. Simple soap and running water do a good job of removing potentially infectious germs.
It may also be helpful to avoid contact with people who show signs of cold or flu. Your doctor may also recommend an annual flu vaccine.
Focus on Good Nutrition
Eating right is an important way to keep your body and your immune system strong. It may be helpful to eat smaller meals, more often. Try to eat a diet rich in fruits, vegetables, fish, nuts, olive oil, and whole grains. Cut back on red meat, sugar, and processed foods. Following this dietary pattern has been shown to help reduce chronic inflammation, while supplying plenty of fibre, antioxidants, and other nutrients to help keep you healthy.
Your doctor may also recommend nutritional supplements to ensure you’re getting the essential nutrients you need.
Tend to Your Emotional Needs
People living with disabling diseases such as COPD occasionally succumb to anxiety, stress, or depression. Be sure to discuss any emotional issues with your doctor as they may be able to prescribe medications to help you cope or also recommend other approaches to help you cope. This might include meditation, special breathing techniques, or joining a support group. Be open with friends and family about your state of mind and your concerns and let them help in any way they can.
Stay Active and Physically Fit
Research shows that exercise training can improve exercise tolerance and improve quality of life among people with mild to moderate COPD. It can also help provide relief from shortness of breath and improve your mental well-being.
Asking for portable oxygen devices from your supplier can aid you in being more mobile and to have oxygen with you whilst you exercise or carry out more strenuous activities.
References: http://www.healthline.com
O-X-Y-G-E-N
O - Options - Ask your supplier for devices or gadgets to help suit you and your home.
X - eXpectations - Medical advancements and oxygen supply companies have come a long way but you should have high expectations for your health, talk to your doctor and make sure you use a reputable, caring oxygen supplier.
Y - Your lifestyle - This can still be maintained with a little oxygen help, especially with portable oxygen devices - keeping active is important!
G - Go on Holiday! - There's no reason why people using oxygen cannot go on holiday, from flights to cruises to mini-breaks abroad by car, just ask your oxygen supplier to help arrange and cater for your oxygen requirements!
E - Enjoy a Long Life! - With improved portable oxygen devices to help you keep mobile and improved medical treatments and drugs, life expectancy has greatly improved and patients live a long, near normal life nowadays.
N - Needs Change - Your disease may improve or worsen or your general fitness may alter and so will your oxygen requirements. Always attend your check-up appointments so that your doctor can alter your oxygen prescription accordingly.
What Would Happen If Oxygen Just Disappeared?

Oxygen is vitally important to us; not just because we need to breath it but because of how versatile and widely used it is:
• Everyone would get sunburnt as oxygen makes up the ozone and normally helps to block out UV light.
• The sky would get darker during the day if there were fewer oxygen molecules to scatter blue light; the sky would appear less blue and more black.
• All engines that use internal combustion would stop working as oxygen is fundamental for combustion.
• All pieces of untreated metal would suddenly weld to one another, as usually the oxidation layer on the metal prevents this.
• Your inner ear would explode as you would lose 21% of the air pressure in an instant, as if you had been suddenly transported to high altitude.
• Any building made of concrete would crumble as oxygen helps to bind all concrete structures.
• Water is one third oxygen, without it the Hydrogen becomes a free gas and expands, thereby destroying all living cells and evaporating the oceans.
• The earth below us would disappear and we would free fall. The earth's crust is made up of oxygen, about 45% so without it the majority of the earth's crust would disappear from beneath our feet.
References: http://www.breathing.com
Tips On Using Supplemental Oxygen With Children
Many babies and young children require oxygen treatment at home, and depending upon the condition this could be for a short period of time or long-term. Here are some tips to help make life a little easier when dealing with oxygen at home.

The nasal cannula that supplies the oxygen to their nose requires fixing securely to the child's face to ensure that the tubing does not become dislodged. Keeping the tubing fixed to a child can be difficult. You can use special cushioning plasters to have under the tubing so that it does not rub the child's face and the fixing tape can be applied over the tubing and stick to these cushioning plasters. Also when you need to re-secure the tubing it means that you won't have to keep pulling tape directly off of the child's skin.
However if your child requires oxygen overnight it is best to use tape directly onto the skin to ensure more secure fixing to the skin in case they move in their sleep and the tubing moves. You can wet the tape warm water or baby lotion though using tissue or cotton wool so that the tape can be removed more easily without pulling your child's skin or causing them discomfort.
Older children may not need the tubing to be taped as the tubing can be looped behind their ears abd the toggle pulled comfortably taught behind their head.
If your child has sensitive skin there are alternative tapes that can be used if your child has eczema or other sensitive or allergic reactions to the normal tape.
The use of petroleum-based creams such as Vaseline around the nose should be avoided as these react with oxygen and may cause soreness, however water based creams such as E45 or KY Jelly can be used instead.
If your child tries to pull the nasal cannula off then ensure that the tapes are secured closer to their nose, rather than on their cheeks and close to their ears to reduce the gap.
As your child gets older they become more active at night and they may wiggle around more. You could put mittens on your child's hands at night to prevent them from being able to tug at the tubing. Also the tubing should be checked so that it doesn't become wrapped around them. To prevent this you can thread the tubing down through their baby-gro or down through their pyjamas so that the tubing comes out by their feet and have the oxygen supply unit at the bottom of their crib or bed.
Some children resist wearing nasal cannulas or face masks and it can sometimes help to let them play with a spare one, to see it on another child or to put it on a favourite stuffed animal or toy. If your child's face becomes irritated by the cannula then try using a face mask instead or the use of a humidifier can keep the oxygen moist and prevent nose irritation from dry air.
Children are very adaptable and may not always let you know when something is wrong therefore you will need to be observant for any changes that may indicate that they are not receiving enough oxygen. Such as them feeling drowsy or tired, morning headaches, shortness of breath, less active, breathing harder or has blue lips or nail beds. If these symptoms appear then you will need to call your doctor. It may just be an indicator that the oxygen rate needs to be adjusted or there may be a medical problem.
References: http://www.alderhey.nhs.uk and http://patients.thoracic.org
How's Best to Chauffeur Your Oxygen Around?!
The wonder of lightweight and portable devices is that you can get out of the house and keep active, however it is medical equipment containing a gas that aids combustion, so safety precautions should be taken for your own safety.

• It is recommended that you carry a copy of your documentation with you such as your Medical Oxygen Data Sheet.
• Inform your car insurance company that you intend to carry oxygen in your car.
• Keep the car well ventilated, open a window and set the ventilation to take in air from outside.
• Do not smoke or allow others in the car to smoke.
• Never transport the liquid oxygen mother unit container in the car.
• If possible carry your spare cylinders securely in the boot of the car. Use a cargo net to secure them properly.
• Remember to also secure the ambulatory cylinders or portable liquid flask in your car to prevent any harm coming to passengers or to the vehicle.
• Keep the amount of oxygen that you transport to a minimum and don't transport large, high capacity cylinders in the car.
• Instead of placing the equipment loose on the back seat, strap it into the seat with a seat belt or place securely in the foot well in the back.
In summary remember that if loose the equipment could shift or move and damage the car, the passengers or the equipment itself so secure it well.
Also due to oxygen's ability to aid combustion you need to keep the car well-ventilated in case of a leak to prevent a build-up of the gas within the car and to not smoke around it.
Carry documentation in case of an accident as if you are unconscious the emergency services could then be made aware of it's presence and also of your medical need for oxygen which could save your life.
References: http://www.bochealthcare.co.uk
Which Oxygen Breathing System Is Best For Me?
Nasal Cannulas
Nasal Cannulas tend to be popular as they can be used for their simplicity and patient convenience.
Nasal Cannula prevents re-breathing of expired air and are comfortable for long periods of time.
There is increased patient compliance with a nasal cannula as patients are able to speak, eat and drink more easily as the mouth isn't covered. It is smaller and more discrete and patient's are more likely to wear it continuously.
Local irritation and dermatitis may occur if you are being prescribed a high flow rate of oxygen. The use of humidified oxygen is recommended with its use to reduce the dryness of the mucosal wall in the nasal cavities, particularly when using flows of greater than 4 l/min. They can withstand flow rates of 1-9 L/min up to 40% oxygen.
If you want to move around a lot some patients find that the tubing can slip off from around the ears or that they can rub the cheeks and ears, although special tube cushioning can be supplied to reduce this.
Face masks

Many patients prefer the traditional face mask.
There are a few different types of face masks but the basic principle is the same. They deliver a higher rate of oxygen than cannulas; up to 15 L/min of oxygen and up to 60% oxygen concentration, depending upon the patient's breathing and tidal volume.
They are normally soft and mould easily to the face, although they should be fitted to ensure that they do fit your face properly and that there are no gaps where the mask doesn't meet the face properly as the oxygen will escape through these gaps.
They have head straps or ear loops to allow easy fitting and removal. The clear ones allow others to visually spot any indications that you are in difficulty.
Most masks are careful to direct the oxygen directly into the nostrils and not upwards towards the eyes which can cause eye irritation. Some face masks have a horizontal tube to further reduce this risk.
References: http://www.flexicare.com and http://www.christie.nhs.uk