The ABC's of COPD
The ABCs of COPD
COPD is a catch-all term for bronchitis, emphysema and in some cases, chronic asthma. All are associated with airflow obstruction, says Andrew Ries, a professor of family medicine and preventive medicine at the University of California--San Diego. While some patients have a lot of coughing and phlegm, breathlessness is the red-flag symptom. "Patients often first notice it with activities -- they're getting older, and they can't keep up with people their own age on inclines or stairs," Ries says. "They're getting more shortness of breath, and their physical activities are getting diminished -- and it's more than just aging."
There's no cure for COPDs. The goal is to slow progression as much as possible to maintain quality of life and keep patients from getting worse.
"C" Is for Cigarettes
About 15 million Americans have been diagnosed with COPD, while millions more may have it without realizing it. It's the third leading cause of death in the United States and a major cause of disability, according to the Centers for Disease Control and Prevention.
Heavy smoking is the common denominator. At least 80 percent of COPD patients are current or former smokers, usually with pack-a-day (or more) habits over many years. Many people struggling with COPD now were kids or teens when the landmark U.S. Surgeon General's report on the health risks of smoking came out 50 years ago. Back then, smoking was still popular and becoming more so among women. However, COPD is not always due to smoking. A genetic condition called alpha-1 antitrypsin deficiency -- a lack of a lung-protective enzyme -- puts people at higher risk for COPD, specifically, emphysema.
Similar to lung cancer, death rates from COPD are declining -- at least in men. From 1999 to 2010, death rates dropped from 57 men per 100,000 men to less than 48 per 100,000, according to the CDC . But rates for women increased slightly in the same period -- from about 35 to 36 women per 100,000 women.
"O" Is for Oxygen
Tony Kanzia, 68, has COPD, which nudged him into retirement. After working in the automobile industry in the Chicago area for 35 years, he called it quits. "I couldn't do my job anymore," he says. "I couldn't even walk out to the lot to show people the car; let alone go on a test drive -- I needed my oxygen."
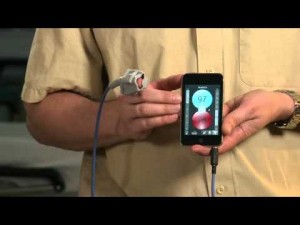
He used to enjoy air travel but the planning -- let alone the flights -- all became too much. It involved calling the airline in advance and renting an oxygen tank, along with packing his pulse oximeter -- a small device that lets people clip a probe on their finger or ear to show how well blood is saturated with oxygen. Kanzia recalls the last straw flight, when even a trip to the restroom became a hazard. To tolerate the expected minute or two without his oxygen, he did breathing exercises before leaving his seat. But when he exited the restroom, the service cart was blocking the aisle, and his oxygen saturation dropped as he waited. Flight attendants saw he was in distress and got him back in his seat.
Many COPD patients manage without oxygen therapy, or only use it as needed. Others with severe COPD rely more heavily on oxygen.
Jean Rommes, 70, a semi-retired consultant and COPD activist in West Des Moines, Iowa, still travels a lot -- always with an oxygen tank. Her strategy is to "swallow her pride" and get help as needed to save precious energy. She flies via major airports and uses a wheelchair to get from one concourse to another, although she prefers going by an airport cart with other travelers.
Bunny Music, 70, of Sussex, New Jersey, has used oxygen around the clock for 13 years. She uses liquid oxygen, which she finds easy to carry over her shoulder, rather than a cumbersome gas cylinder (the green tank on wheels). Oxygen concentrators are the third option, but Music says they're heavy and hard to manage with a walker or cane, and "you can't depend upon them if your electricity goes off."
"P" Is for Progressive
To experience how it feels to have COPD, plug your nose and then put a straw in your mouth and try breathing through that, suggests Janet Shaw, 66, of Glendale, Arizona. "That'll give you an idea of what it's like -- and that's on good days," she says with a laugh. "On bad days, it's harder to breathe."
In healthy lungs, the air sacs and airways are elastic. Each time you inhale, the air sacs fill up with oxygen and then deflate as you exhale carbon dioxide waste. But with COPD, this elastic quality is lost, and walls between the airways become damaged, thick and inflamed. Narrowed airways can become even more obstructed with dense, excess mucus, making breathing even harder.
For someone who starts smoking as a teen and persists into adulthood, damage can go on quietly for years, Ries says. "Because you have two lungs and a lot of lung reserve, most lung diseases really don't cause significant problems or symptoms until someone has lost 50 or 60 percent of their lung function." Then a respiratory problem, even a cold, "pushes them over the age, and that's in their 50s, 60s and 70s."
Pneumonia and other respiratory infections often cause symptoms to flare, and COPD care includes keeping up with flu and pneumonia vaccinations.
Early intervention is crucial in staving off COPD progression -- so even if you've never been diagnosed with COPD, but are having breathlessness or other ongoing respiratory problems, it's worth going to a doctor to be screened. You'll likely be given a spirometry test -- a noninvasive way to measure lung function. "Anyone who's got any kind of problem, or is a smoker, [should] see a doctor and get a spirometry test and find out if you have obstruction," Ries says.
"D" Is for Dealing With It
People with COPD can cope by taking prescription medications, keeping up with treatments, building endurance through exercise, accepting limitations and making adaptations in their homes, like rearranging kitchens so they can sit while preparing food. Many use inhalers with drugs called bronchodilators, like Spiriva, to relax muscles in the lungs and widen the airways. Some people also use inhalers that combine a bronchodilator with a corticosteroid to reduce inflammation -- such as Advair and Symbicort.
Lung reduction surgery is sometimes used in severe cases of emphysema. "The surgeons can go in and take out over-expanded parts of the lung, and buy some improvement in symptoms and function for a limited number of patients," Ries explains. For the most severe COPD, lung transplant is an option to improve function, but it's not a cure.
It's possible -- and important -- to build fitness and endurance if you have COPD, says Ries, also the director of the Pulmonary Rehabilitation Program at UCSD. "One of the cornerstones of rehabilitation efforts is getting people to be physically active," he says, "because they often get very sedentary because they're so short of breath."
For her part, Hinkle swears by the UCSD program, which she started in June. Now she tries to make it to the gym to walk on the treadmill three days a week, and she's ramping up her speed and intensity. She's also been introduced to weight machines that will help build up her core strength to support her breathing.
Kanzia's motto for living with COPD is "improvise and overcome." He uses an oxygen concentrator with a 50-foot cord so he can move around his house, and his kitchen is organized for success. "I do a lot of cooking, no problem," he says. "I make a great bowl of spaghetti." Last week he took his grandchildren to the zoo, with the help of other family members and a portable electric scooter.
Hinkle says necessity has taught her the importance of "recognizing when you need help with things and getting it." She strives to remain as self-sufficient as possible -- while taking care of her elderly father. She continues to gain support and encouragement from other members of her pulmonary rehab group. "It's nice to know you're not the only one with these problems," she says, "regardless of what caused them."
Lisa Esposito is a Patient Advice reporter at U.S. News. You can follow her on Twitter, connect with her on LinkedIn or email her at lesposito@usnews.com.
Oxygen and cluster headaches
Oxygen Inhalation for Cluster Headaches
Oxygen is given at a high flow rate of 6 to 7 liters a minute for 10 to 20 minutes at the start of a cluster headache.
High-flow oxygen inhalation therapy is used to treat cluster headaches. If headache pain is not relieved within 20 minutes, oxygen therapy should be stopped.
High-flow oxygen therapy does not prevent a cluster headache. It only provides temporary relief of headache pain.
Oxygen therapy is one of the best treatments to stop a cluster headache. Oxygen therapy relieves headache pain within 15 minutes in more than 7 out of 10 people who use it. It works best when started right when a cluster headache starts.
In general, there are no adverse effects from oxygen treatment. But oxygen is a fire hazard. It is important to follow safety measures to keep you and your family safe. Do not use oxygen around lit cigarettes, open flames, or flammable substances.
Your doctor will set the flow rate per minute to give you the right amount of oxygen. Don't change the flow rate unless your doctor tells you to.
If needed, oxygen can be combined with cluster headache medicines (such as sumatriptan) for the most effective treatment. Oxygen also may be combined with preventive medicines to reduce how often you get headaches.
References:
(Cohen AS, et al. (2009). High-flow oxygen for treatment of cluster headache: A randomized trial. JAMA, 302(22): 2451–2457)
New App Measures Blood Oxygen Levels using Smartphones, Tablets and Laptops
A great article below posting about technology advances and Oxygen.
When ET's finger pulsed red it was a sign that he was alive and well. Steven Spielberg probably got the idea for this from seeing pulse oximeters at work. With my daughter's heart disease I became very familiar with this important indicator of wellness.
Pulse oximeters measure oxygen saturation in the blood. They do this by taking advantage of the light absorptive capability of hemoglobin. When attached to a finger the device tracks blood from each pulse or heartbeat as it passes by the light sensor. A pulse oximeter houses an infrared and red light generator, a light detector and a microprocessor. The greater amount of infrared light absorbed by the light detector the higher the oxygen saturation reading. On room air a reading in the high 90s is most desirable. Lower readings indicate compromised airways, pneumonia, heart disease and many other medical conditions one of which is preeclampsia, a condition that causes high blood pressure during pregnancy and often can lead to death for the mother and infant if not detected early.
Pulse oximeters are readily available in Developed World hospitals but not so much in the Developing World. Hence a group of scientists at the University of British Columbia came up with an alternative. With funding from the Canadian government and private investors they developed what they are calling the Phone Oximeter, a $40 device that takes pulse oximetry out of the hospital and makes medical-grade diagnostics possible anywhere. A standard medical sensor connects to the audio port of virtually any mobile device. It can be used with tablets, laptops and smartphones.
With preeclampsia killing 76,000 pregnant woman every year and more than 500,000 unborn or newborn children, and with 99% of these deaths occurring in the Developing World the Phone Oximeter is about to begin medical trials targeting 80,000 pregnant women in India, Pakistan, Mozambique and Nigeria.
Breathing an idea to life: Injectable oxygen microparticles
An amazing article by John Kheir on June 27, 2012 please read below...
John Kheir, MD, is a staff physician and researcher in the Cardiac Intensive Care Unit at Boston Children’s Hospital. As reported this week in Science Translational Medicine, he led a team that created a method for IV oxygen delivery — tiny particles filled with oxygen gas, mixed with liquid and injected directly into the blood. In an emergency, the injections could potentially buy clinicians time to start life-saving therapies. The technology was reported by The Atlantic, Popular Science, Scientific American, Technology Review and other outlets.
It was an ordinary Saturday night in the ICU at Boston Children’s, in the fall of 2006. One of my patients was a 9-month-old girl who was admitted with pneumonia, and was having trouble breathing. I had gone in to check on her just a few minutes before; although she was not feeling well, she reached out and touched my hand as I examined her. I assured her mother she was in the best possible place for her care.
Five minutes later, the code bell alarmed. Our team rushed into her room to the most horrific sight I have ever seen. She lay limp in bed, lifeless. Her face was covered in blood, which we knew came from her lungs. We rushed into position.
My colleague and I placed a breathing tube, while the nursing team performed CPR and administered all of the proper medications. The tube was in the right place, the medications were getting in, everything was happening right on time… but she remained lifeless.
Her oxygen saturation was too low for her to resuscitate, so we decided to put her on a heart-lung bypass machine. This procedure is technically challenging under any circumstances, but here especially when we were performing CPR. Although we were able to get her onto the machine, and her heart was revived, we learned once again the lesson that ICU clinicians hate: The brain is the most sensitive organ to low oxygen delivery. She was no longer the person she could have become. It had all been taken away from her in the 20 minutes her brain was deprived of oxygen. She died three days later.
I was devastated and frustrated. We did everything exactly right. I lay in my bed that night staring at the ceiling. She could not have received better care, and yet she still died. What good was our amazing technology if patients are so injured by the time they are effectively supported?
At the time, I was a fellow – early in my career. I didn’t really know the first thing about research, but I knew that this was a big problem that nobody had an answer for. Why couldn’t we just make a form of oxygen that we could inject into an intravenous line? I found that there was a whole field of research focusing on gas-filled microbubbles that people used for ultrasound contrast agents and for targeted therapy. Maybe we could alter that technology to be able to safely inject oxygen gas.
I had an idea, but no concept of how to approach it. I didn’t have a lab, or money, or a mentor. But the first thing I learned is that inspiration is the sine qua non of important research. Then, I was immensely blessed to find a mentor who took on this ragamuffin researcher with a crazy idea. I met with Frank McGowan, MD, the then-Chief of Cardiac Anesthesia at Boston Children’s — a highly accomplished researcher with nothing to gain (and a lot to lose) from me. But he took me in, met with me often, gave me space in his lab, taught me how to do research, how to write grants and papers, and how to test my ideas in a rigorous way… every essential research skill.
Although we had every likelihood of failure, he took a risk on me. And that is the second lesson I learned: that nothing good ever happens without taking a risk. True accomplishment is what you accomplish when nobody else believes in what you are doing.
The first experiment I remember was the simplest one we performed. It was a Friday evening, and my mentor was stuck in the operating room. I met him there with a vial of test suspension that my colleague, Mark Borden, PhD, had sent me. During a break, Dr. McGowan drew my blood, and we mixed it with the microparticles. We watched my blood turn from blue to red — indicating that the microparticles had successfully transferred the oxygen to the blood. That success was followed by hundreds of failures… blood that did not turn red, problems manufacturing the microparticles, and animals who did not survive even brief injections.
The idea of injecting oxygen into a patient is possibly now less far-fetched than it was six years ago. We have many obstacles to overcome to bring this idea to a patient’s bedside. But even if it never happens, I would rather have tried and failed than to have just turned over in bed that night and said, “that’s too bad… we tried everything.”
Hear more in this podcast.
Respiratory Devices Market 2018 Global Analysis and Forecasts
'The increasing adoption of portable respiratory devices market by patients makes them feel better and improves their quality of life.' Portable Respiratory Devices Market 2018 Global Analysis and Forecasts A good read: http://lnkd.in/bpnxftT

What is a portable oxygen concentrator?
An oxygen concentrator is a device which concentrates the oxygen from a gas supply (typically ambient air) to supply an oxygen enriched gas mixture
 Oxygen concentrators typically use pressure swing adsorption technology and are used very widely for oxygen provision in healthcare applications, especially where liquid or pressurised oxygen is too dangerous or inconvenient, such as in homes or in portable clinics.
Oxygen concentrators typically use pressure swing adsorption technology and are used very widely for oxygen provision in healthcare applications, especially where liquid or pressurised oxygen is too dangerous or inconvenient, such as in homes or in portable clinics.
Oxygen concentrators are also used to provide an economical source of oxygen in industrial processes, and also known as Oxygen Gas Generators or Oxygen Generation Plants
An oxygen concentrator has an air compressor, two cylinders filled with zeolite pellets, a pressure equalizing reservoir, and some valves and tubes. In the first half-cycle the first cylinder receives air from the compressor, which lasts about 3 seconds.
(wikipedia,2014)
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is the name for a collection of lung diseases including chronic bronchitis, emphysema and chronic obstructive airways disease. (NHS direct)

Typical symptoms of COPD include:
- increasing breathlessness when active
- a persistent cough with phlegm
- frequent chest infections
Oxygen therapy can help! In fact, getting oxygen can prevent all those bad effects that happen when blood oxygen levels drop. Oxygen can reduce the strain on your heart. Oxygen can reduce shortness of breath. It will help you to stay more active and exercise longer and harder. It will help you think and remember better. And it will help you sleep better. Oxygen therapy CAN make a big difference in how you feel.
Oxygen therapy is a medical treatment. It must be prescribed by a doctor. For people with COPD, oxygen therapy can be a helpful part of their treatment plan. The prescription your doctor writes will include:
- If you need oxygen for rest, exercise and/or sleep, and how much in liters per minute (lpm) for each activity.
- How many hours a day oxygen should be used.
- What type of oxygen system you should use.
COPD is one of the most common respiratory diseases in the UK. It usually affects people over the age of 35, although most people are not diagnosed until they are in their fifties.
It is thought there are over 3 million people living with the disease in the UK, of which only about 900,000 have been diagnosed. This is because many people who develop symptoms of COPD do not get medical help because they often dismiss their symptoms as a ‘smoker’s cough’.
COPD affects more men than women, although rates in women are increasing.
Find out more about our services using medical oxygen www.oxygenworldwide.com
Portable oxygen
The first thing that you should consider when purchasing one of these is durability. This actually means two different things. Durability can be talking about the physical housing and how well it stands up to bangs, bumps, and drops. After all, this is a portable unit, designed to be on the move, and therefore much more prone to accidents that could prove very difficult to handle, especially in an emergency. A strong casing and carrier are absolute musts.
However, durability can also refer to battery life. A portable oxygen concentrator is an electronic device and therefore need to be either plugged into an outlet or be running on battery power in order to work. Ideally, the longer the battery life, the less you have to worry about being without oxygen while out and about. Most portable oxygen concentrators these days have battery lives in the range of six to ten hours of use with a double battery, though advancing technology predicts that soon we’ll have batteries that can power a typical concentrator for twelve or sixteen hours, perhaps even longer.
Size and weight should also play a large part in which portable oxygen concentrator you consider buying. In this case, smaller and lighter concentrators tend to be better. They are “portable”, after all, and a 17 pound device is not nearly as easy to tote about town as one might expect. Portable models are getting lighter and smaller all the time, and many these days weigh as little as eight, five, or even three pounds. There was a time not very long ago that the very idea of such a light unit was absolutely unheard of.
There aren’t a whole lot of factors to consider, but all of them are very important. This is a medical device that for many people is the difference between life and death while running errands, visiting friends and family, or just taking a walk. The ability to carry it comfortably and trust that it will work when it’s needed is absolutely key to any such purchase.