Stopping smoking will not only help your lungs, but also your brain!
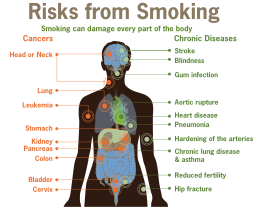
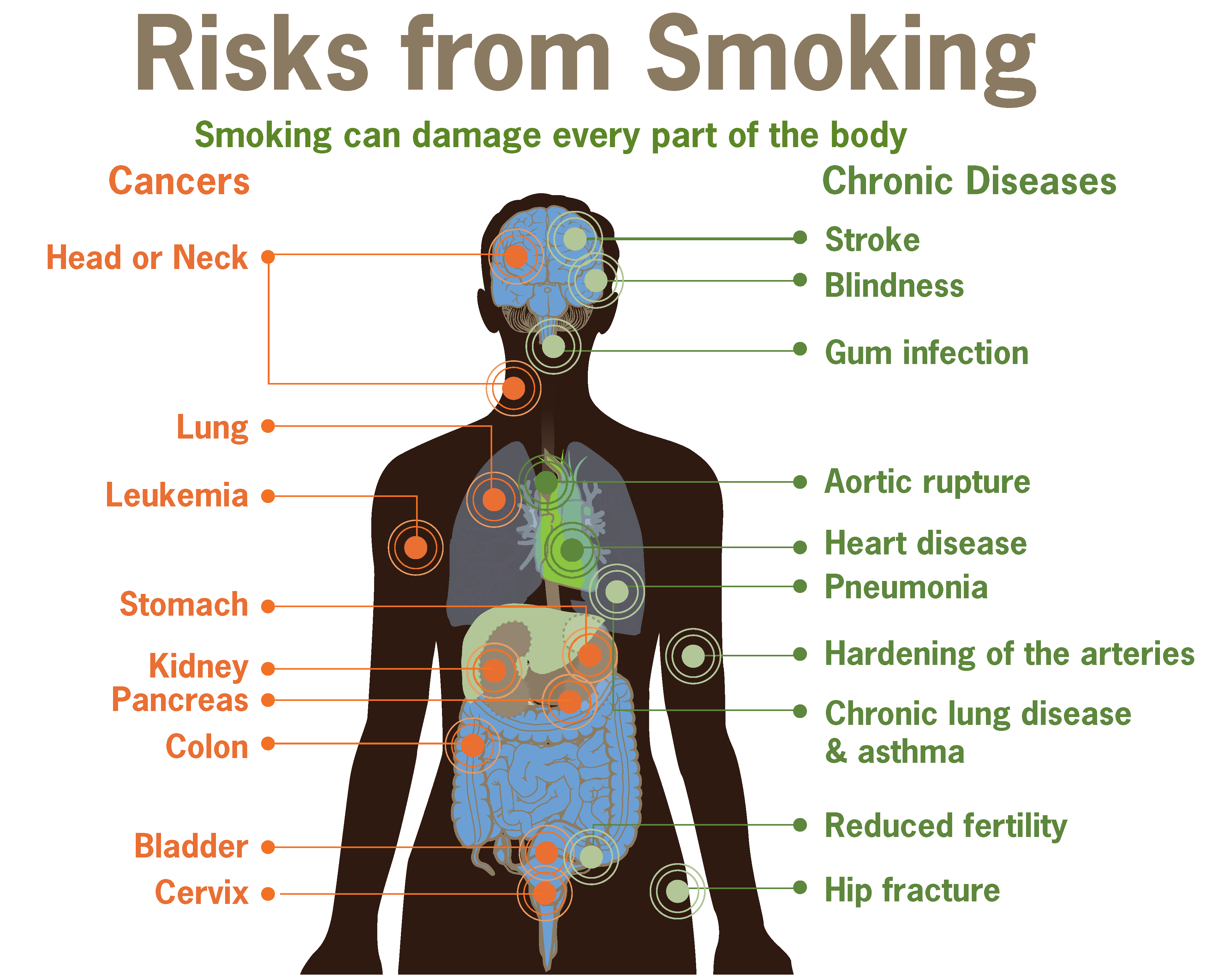
For COPD patients and others that use supplemental oxygen to help them to breathe, quitting smoking is hugely important to stop further lung damage, help slow the disease down and reduces the danger of smoking near oxygen cylinders. 2016 is going to be the year to stop smoking as part of a new campaign to try and combat lung disease. However if you stop smoking it is not only your lungs that you will help but your brain will benefit too.
It's never too late to quit, even if you're in your 70's, there is still a chance for a noticeable recovery. For light smokers the damage can be reversed in a few weeks and for heavier long-term smokers it may take anywhere up to 25years for full recovery but every little helps.
The cerebral cortex, which is responsible for memory, attention, awareness and language naturally thins with age but this process is hugely accelerated by smoking. Scientists at the University of Edinburgh found that even though smoking thins the outer layer of the brain and increases the risk of memory problems and dementia, it is reversible. The damage that cigarettes cause to the brain can start reversing as soon as you give up the habit. Even when quitting later in life there is still a chance of reversing the harmful damage done to your brain.
In the study the thickness of the cerebral cortex was measured and important thinking skills were tested on smokers, non-smokers and ex-smokers. Those who had never smoked tended to have a thicker cortex than the smokers but ex-smokers also had a thicker cortex than those who had continued with the habit. Also more importantly those who had kicked the habit some time ago seemed to have a thicker cortex than more recent quitters, showing that there had been continuous recovery.
Professor James Goodwin from AgeUK talks about how we all know that smoking is bad for our heart and lungs but it is also important that we know it is also bad for our brain. Avoiding smoking offers the best protection against the risk of brain decline, dementia and other cognitive disease but this study gives smokers a new hope that by quitting smoking even later in life can still allow our bodies to start to heal itself.
“With research suggesting that older people’s fear of developing dementia outweighs that of cancer, it is important we inform people about the simple steps they can take to safeguard against this horrible and distressing disease.”
COPD patients already have many health issues related to their condition but the fear of cancer and dementia adding to them is concerning for patients. Knowing that by quitting smoking you can help to reverse damage to your brain, on top of preventing further damage to your heart and lungs, reduce the risk of combustion with oxygen cylinders and concentrators and halting progression of the respiratory disease you're suffering from is a huge incentive for people to encourage them to give up smoking.
References: http://www.dailymail.co.uk
E-CIGS: Worth it?!
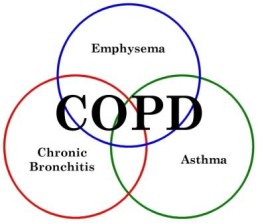
Smoking is the main factor in developing COPD and many patients struggle with giving up smoking. E-cigarettes could be the way to help COPD give up and to improve their lung function and slow down the progression of their disease. Using oxygen to help improve your breathing is highly beneficial in coping with the disease but if you are still smoking then it is counter-acting the good work of the oxygen and other medications prescribed for you. However what are the facts and are they actually safe?

Electronic cigarettes are battery-powered devices filled with liquid nicotine that is dissolved in a solution of water and propylene glycol. They can look very similar to ordinary cigarettes or other designs are less conspicuous. Often termed as 'vaping' you take a puff, the battery heats up the nicotine which creates a vapour than you then inhale, resulting in a sensation similar to smoking but without the smoke.
You can smoke them indoors, they are closer to a nicorette inhaler than tobacco and there are many studies supporting the opinion that they do alleviate the desire to smoke. For those people that use them in conjunction with tobacco in order to cut down on their tobacco intake, they found that they managed to reduce their tobacco intake and not suffer from any withdrawal symptoms. They have worked for people who constantly fail at ceasing smoking via other conventional methods. An online survey revealed that 96% said that E-Cigarettes helped them to quit smoking, 92% said that it made them smoke less and the majority stated that they helped to fight cravings, cope with withdrawal symptoms and avoid relapsing.
However many feel that they are not regulated enough and lack essential health warnings, proper labeling and instructions and disposal methods. Some have been found to leak which may expose you to a toxic exposure of nicotine.
A study found that e-cigarettes caused accused pulmonary effects after smoking it for 5 mins. Healthy non-smokers were reported to suffer airway flow resistance and oxidative stress. The authors however also suggested that if they were only being used as a bridge to stop smoking then the benefits would outweigh the risks.
The FDA states that "E-cigarettes may contain ingredients that are known to be toxic to humans, and may contain other ingredients that may not be safe." They also suggest that because e-cigarette manufacturers are not required to submit clinical study data to them, the public has no way of knowing "whether e-cigarettes are safe for their intended use, what types or concentrations of potentially harmful chemicals are found in these products, or how much nicotine they are inhaling when they use these products." The FDA is also concerned that the marketing efforts of e-cigarettes may increase addiction to nicotine, especially in young people, encouraging them to experiment with real tobacco products.
It is important to stop smoking as a COPD patient, not only for your health but for your safety due to the use of supplemental oxygen and the dangers of smoking around oxygen tanks. However how you choose to quit is a matter of personal choice and everyone is different and will respond differently to the various methods that are available from nicotine gum/patches, quit smoking medications, support groups and educational materials as well as E-cigarettes. You have to decide what is safe and easiest for you and ask your doctor for help, advice and support.
References: www.jsonline.com and http://copd.about.com and www.dailymail.co.uk
Image Credit to www.vaping360.com
COPD muscle weakness and the importance of oxygen
It has recently become apparent that patients with COPD commonly suffer skeletal muscle dysfunction, which may be the main cause in the reduction in exercise tolerance.
COPD patients tend to reduce their levels of physical activity as it causes unpleasant effects and results in a vicious cycle where a reduction in physical fitness leads to further impairment of muscle function
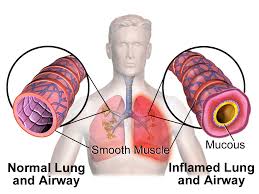
Skeletal muscle dysfunction is very common in patients with COPD, and may play an important role in limiting exercise performance. Muscle strength and endurance are both decreased and the muscle is more easily fatigued. Muscle atrophy is largely responsible for the reduction in muscle strength but deconditioning is of major importance as well as nutritional depletion, and steroid use. COPD may also produce a systemic inflammatory response that may adversely affect skeletal muscle function.
Muscle strength is seen to be decreased in patients with COPD and particularly in the lower limbs. An important factor is muscle wastage; either through medical reasons or a lack of exercise due to breathlessness. Muscle endurance and the length of time the muscles can be used also decreases significantly. In biopsies the ratio of different muscle fiber types are altered in COPD patients and type IIa convert to type IIb, resulting in reduced muscle endurance, increased fatigue and a reduction in muscle mass. The number of capillaries within the muscle is also significantly lower in COPD patients as well as the number of mitochondria. Enzymes that are required for metabolism within the muscles are also decreased in COPD patients. This all results in less oxygen reaching the muscle cells and metabolism and function of the cells being adversely affected.
Medications such as steroids which are used to treat exacerbations can also cause muscle wastage. Short-course doses are beneficial to the patient but long-term multiple short-courses requires further study.
Malnutrition is also common with COPD where 35% are less than 90% of their ideal body weight. This results in a reduction in muscle mass and metabolic functions are disrupted. Nutritional supplements however are not a substitute for eating a balanced, healthy and high in calories food plan. Patients can tend to either put on weight from a lack of mobility or lose weight from the increased energy required to breath and a reduction in appetite due to the difficulty of eating and breathing with breathlessness and the need for constant oxygen supplementation.
Deconditioning from disuse is believed to be the major contributing factor in the skeletal muscle dysfunction observed in patients with COPD. When healthy individuals undergo a training program to increase fitness levels physiological and morphological changes are seen and results in muscle larger in mass with increased oxidative capacity and more efficient in its ability. From previous studies it was thought that COPD patients could not reach the same levels of increased muscle efficiency when undergoing the same training program. However studies have shown that a certain level of intensity and duration needs to be reached before the muscle will begin to improve.
Exercise training will improve skeletal muscle function in those with COPD and pulmonary rehabilitation is shown to improve endurance capacity and quality of life, however the type of exercise training should be further studied and bespoke personal exercise plans developed for individuals to to get the maximum potential from their exercise.
Oxygen therapy is provided for patients to help them to breathe but long-term oxygen therapy has been shown to help improve muscle function and metabolism. It also reduces the potential harm of deconditioning as patients on oxygen therapy tend to be more mobile and physically active as they benefit from the positive benefits of supplemental oxygen.
Muscles require constant use, a balanced supply of metabolites from our diet and oxygen in order to work efficiently. Studies have shown that oxygen therapy not only directly affects muscle function positively but it enables patients to be more physically active and exercise more frequently and for longer, which in turn reduces potential deconditioning and helps to build up muscle mass, strength and efficiency.
REFERENCES: www.ncbi.nlm.nih.gov and www.respiratory-research.com
Could lung coils be the new treatment for COPD?
A recent trial has shown that the use of lung coils has produced significant lung function improvements for emphysema patients.
In advanced emphysema parts of the lung become hyperinflated when patients breathe in and these can press down on and impair the healthy lung tissue as well as pushing down on the diaphragm making breathing extremely difficult. Patients would normally undergo surgery and have a lung-reduction procedure, however this is risky and very invasive. The new lung coil may offer a less invasive and effective alternative treatment to reduce lung volume.
The coils are shaped in a simple loop around 10-15cm in length when stretched out. They are made from Nitinol which is a metallic 'memory' material that returns to its intended shape even after long-term repeated stretches and compressions.
They are inserted into the lungs using a bronchoscope and placed in areas with diseased lung tissue where they immediately resume their looped form. The coils grab lung tissue and pull it inwards to reduce the lung volume in these sections to allow other sections with healthy lung tissue to inflate more normally. It has been shown that a minimum of 10 coils are needed in order for there to be significant clinical benefits but 12 per lung is the current practice.
Coil treatment has shown to provide significant improvements in the 6 min walking distance test and forced expiratory volume and also less dependence on supplemental oxygen. These results are from 3 months post coil insertion and the trial is still continuing for another 9 months to see if the good results continue long-term. If the results continue to show an improvement in lung function and breathing ability long-term then the coil treatment will be an effective new treatment for COPD patients and other patients with diseases where damaged lung sections cause difficulty in breathing. It is far less drastic and invasive than lung reduction surgery and results show that it is more effective.
References: http://www.medpagetoday.com
Working with COPD
COPD can have a devastating impact upon your personal life but if you are also aged 45-65 it can also have an even greater impact on your job. Work-loss for COPD patients is not just due to COPD alone but also due to the other associated medical problems that coexist with COPD. Not being able to work has an impact on the rest of your life, from financial worries to personal fulfillment.
Results from a cross-sectional survey of 2,426 people with COPD living and working in 6 countries around the world (Brazil, China, Germany, Turkey, United States and United Kingdom) revealed the following:
• 80% were unable to maintain their previous lifestyle.
• One in four felt they could not continue to care for their children or other members of their family as they once did.
• One in five felt they had become a burden to family members and friends.
• 41% felt they could no longer plan for their future.
• 37% reported their income had dropped since being diagnosed.
However some people still manage to continue working until retirement. It depends on your job role; will it make your condition worse by continuing to work in that role or is there an option to change roles or career so that you can still work? If this is not possible then you can claim long-term disability which will give you some income.
If however you feel that you can continue employment then there are things that you and your employer can do to make your work life less of a burden on your disease. The employer will welcome that a few changes will help to ensure that you don't take as many days off from work for being ill.
Here are just a few accommodations that employers can make that are not overly imposing:
• Providing an accessible parking space that is close to the door.
• Moving your workstation closer to the entrance of the building.
• Allowing you to work from home at least a couple of days a week, if not every day.
• Providing a smoke-free, dust-free, fume-free environment. This can even mean asking other employees not to wear heavy colognes or perfumes.
• Providing adequate ventilation.
• Allowing you a flexible schedule so that you don't miss your doctor appointments or perhaps letting you come in later on certain days.
• Giving you advanced notification of any construction work or cleaning that will be going on in your particular work area.
• Allowing you to use a scooter or motorized cart to increase your mobility while in the workplace or to move from one office building to the next during work hours.
If your employer makes changes to help you then you must try to ensure that you are as productive as possible in return:
• Doing everything you can to prevent COPD exacerbation. An exacerbation can cause you to miss more days of work, or worse yet, land you in the hospital. Frequent hand-washing, staying away from crowds and sick people and getting your vaccinations will all help.
• Wearing your oxygen at work. Oxygen therapy helps prevent breathlessness, improves your mental alertness and increases your stamina so you can get through your work day. If you feel conspicuous with your nasal canula then there are oxygen glasses you can try or tracheal oxygen may be an option as you can hide the tubes with a scarf or a high-neckline top.
People with COPD are more likely to accept early retirement than those who do not have COPD and this can negatively impact your pension benefits and have a dramatic affect on your financial well-being, as well as that of your family.
Before deciding on retirement you should ensure you have explored with your doctor and your employer all possible avenues of adapting your workplace environment and tried different medications before giving up on work completely. You can also talk to a financial adviser to see what else you could do to ensure that you and your family are well taken care of.
References: http://copd.about.com
Fish oil and its far reaching health benefits
Recent studies have shown that fish oil and fish oil supplements provide nutritional protection against some of the most dreaded diseases of aging. Its major power is its ability to stop inflammation which is a key problem in many diseases and most age-related illnesses.

It is well known that a diet rich in omega-3s helps to reduce inflammation but now it has been realised how it happens. While studying acute inflammation in animals, scientists noticed the production of small molecules released in response to inflammation, especially in the presence of high levels of omega-3 fats. “These molecules had a dual set of actions. First, they sent out a 'stop signal,' quickly putting a stop to runaway inflammation. Next, they triggered the active resolution of inflammation.”
If you have a healthy supply of omega-3s in your body then it will help your body to produce these molecules to stop and repair inflammation. This pathway involving these pro-resolution molecules works well with acute inflammation but with chronic inflammation there is a reduced level of pro-resolution molecules which allows the inflammation to keep running at a low active level.
Studies have shown that people with diseases that involve chronic inflammation have reduced levels of pro-resolution molecules. Other studies have revealed that these molecules are sharply reduced with age. “In fact, it is this deficiency that is now recognized as one of the chief reasons that we increasingly suffer from chronic inflammation as we grow older.”
By restoring levels of pro-resolution molecules to normal levels many inflammatory conditions can be resolved and healing can take place. The best way to do this is to ensure you have a healthy supply of omega-3 by ensuring you have fish oil in your diet or take fish oil supplements.
Low-grade inflammation and low levels of these molecules has been linked to excessive body fat, insulin resistance and hypertension. Also boosting levels of these pro-resolution molecules would be especially important to people with cardiovascular disease because they have been found to reduce cholesterol, lower blood pressure, block clot-promoting platelet activation, prevent heart arrhythmias, prevent vascular inflammation and improve vascular function, and protect the heart muscle following a heart attack. “That immense spectrum of action has led some researchers to describe omega-3s as a 'poly-pill,' capable of attacking multiple targets of cardiovascular health at once.”
Lung diseases such as asthma and COPD are well known to involve out-of-control inflammation and recent studies show that asthma sufferers have reduced levels of pro-resolution molecules. Animal studies show that after treatment with omega-3 the asthma attacks were less severe. After a decade it was shown that after fish oil supplementation in pregnant women or the patient there was a 3 fold reduction in allergies and eczema, 63% reduction in children developing asthma, many athletes had a 5-fold improvement in pulmonary function and even non-athletes had vastly improved pulmonary function and exercise-induced asthma became resolved in many. COPD patients experienced significant improvements in their breathing ability, had increased oxygen saturation and found they could walk a lot further.
Neuro-inflammation is a major contributor to chronic neuro-degenerative conditions such as Alzheimer's and Parkinson's. Studies have shown that by increasing pro-resolution molecules derived from fish oil can stop this neuro-inflammation and reduce the cognitive decline in these conditions as well as helping to improve memory and dementia statuses in these patients.
Therefore just by ensuring you are taking in enough fish oil can have a major impact upon your health and can help improve many conditions and diseases that are linked to inflammation.
References: http://www.prohealth.com
3 new treatments for COPD
COPD is a complex disease that is inter-linked with many other diseases and conditions with their own separate symptoms. In order to treat COPD successfully then a range of therapies and treatments is needed in order to combat the disease from all sides.
Recently scientists have discovered three new treatments for COPD patients. Using innovative approaches to help to improve lung function and curb patients' symptoms.
THE COIL:
The lungs can become over-inflated due to trapped air and surgeons have developed tiny coils that can be placed into the lungs to shrink them and restore elasticity. It showed an 18% improvement in lung function after implantation.
“When you release them into the lungs, they just coil up and what they do is they draw the hyper-inflated lung close together,” said Professor of Medicine, at The Cleveland Clinic.
Patients still usually require supplemental oxygen however the coils provide much needed relief and the patient can take deeper breaths and not rely on the oxygen as much.
THE FLUTE:
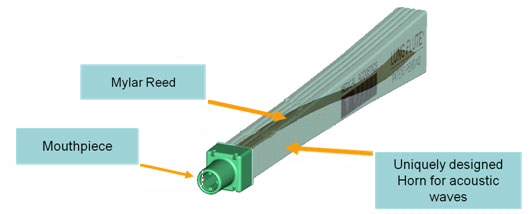
The second new COPD treatment is the Lung Flute, a medical device that improves lung congestion and clears mucus build-up if used twice a day, leading to higher quality of life among patients.
The Lung Flute technology produces low-frequency acoustic waves when the COPD patient blows into it. The acoustic waves are designed to reverberate into the lower airways to loosen secretions that are lodged deep in the lungs. The Lung Flute has been tested in clinical trials and is approved by FDA as a safe and effective form of treatment for COPD.
NEW DRUG:
There is also a new drug called azithromycin which is an antibiotic that has been found to considerably reduce the frequency and severity of flare-ups in COPD patients, if taken long-term, by 20%. The same approach of taking similar drugs long-term has also worked for other lung conditions such as cystic fibrosis. Rather than taking anti-inflammatories or antibiotics reactively after a bad spell, instead doctors use the drugs as preventative treatments and by taking them long-term they build-up and it helps to ease and reduce symptoms.
Depending upon your condition, its status and other medical conditions will mean that each COPD patients has a different set of symptoms and degree of severity and therefore by prioritising the worst symptoms and treating them with different approaches could greatly reduce many different symptoms and greatly improve their condition and quality of life. Ask your GP about different possible treatments and therapies and you may be able to get these products in the private market as they are more and more widely becoming available globally.
References: http://lungdiseasenews.com
WHAT'S THE BEST TREATMENT FOR SLEEP APNOEA?
For those suffering from respiratory diseases, sleep apnoea is often an accompanying condition. Sleep apnoea is a common and chronic condition in which breathing stops or becomes shallow during sleep. Breathing pauses can last from a few seconds to minutes and can occur 30 or more times an hour. Disrupted sleep and a reduction in the level of oxygen reaching the brain can increase blood pressure (leading to heart disease), reduce mental ability and leave you feeling tired and fatigued, in addition to your daily respiratory symptoms.
There are two common treatments for sleep apnoea; continuous positive airway pressure (CPAP) and mandibular advancement devices (MADs). A recent study has shown that both treatments not only are effective in reducing sleepiness and increasing oxygen levels while you sleep but also result in a lowering of both systolic and diastolic blood pressure rates.
MADs work by pushing the jaw and tongue forward to keep the airway open during sleep and are shaped similar to a gum shield. With CPAP the patient wears a mask connected to a device that produces mild air pressure and provides oxygen which helps to keep the airway open.
Some patients find it difficult to adapt to CPAP with problems wearing the face mask or being unable to sleep due to the noise of the compressor and find MADs a more suitable treatment but it does depend on what type of sleep apnoea you suffer from as to which treatment is more suitable.
In the study of 5000 patients both treatments were tested as to their effectiveness and ability to decrease blood pressure. There was no significant difference between CPAP and MADs in lowering blood pressure, they both were equally effective however CPAP was more likely to lower systolic blood pressure compared to MADs and would be slightly more effective in patients who are able to enjoy more hours of sleep.
Even though CPAP appears slightly more effective and are effective across the whole severity range, MADs are equally good as an alternative treatment for some patients who suffer mild to moderate sleep apnoea. The lowering of blood pressure achieved by the two treatments is modest so if you suffer from very high blood pressure you should get it checked regularly and take your medication to help to combat this.
Many patients find that by combating their sleep problems they feel much more able to face the day with their respiratory condition and in combination with oxygen therapy during the day or night they feel able to being able to carry out all their daily activities and feel near normal again.
References: http://www.webmd.com
THOSE WITH COPD MORE LIKELY TO SUFFER FALLS
A recent study has shown that if you suffer from a lung condition such as COPD then you are at a much higher risk to suffer from falls, especially if have other medical conditions, have already taken a tumble or have a long history of smoking.
Past research has already linked COPD to an increased risk of imbalance, muscle weakness, thinning bones and blackouts. COPD alone accounts for 5% deaths globally and falls are also a major public health problem, accounting for more unintended deaths and injuries each year than any other cause (except traffic accidents).
Most falls in the study occurred indoors, often when people were standing and using their upper body at the same time, with loss of balance the most commonly reported cause. It was found that people had more than twice the risk of falling if they suffered from additional medical problems and more than triple if they already had a fall in the previous year. The findings add to growing body of evidence highlighting the increased fall risk faced by COPD patients.
In another study it was also noted that those patients who used supplemental oxygen regularly were at a reduced risk of falls. This is probably due to the fact that oxygen levels are increased in the blood stream due to the use of supplemental oxygen and that the problems such as weakness and imbalance are reduced.
Just one fall especially in the more elderly of patients can result in anything from a bruise to a hip replacement and from an unnecessary trip to the GP or a long-term stay in hospital. Having an injury when you have difficulty breathing only adds to the severity of the injury and the recovery process and could hamper your progress and increase the severity of your condition and lessen your quality of life. COPD patients need to be aware of their increased risk of falling and injuring themselves and take precautions. If you are prescribed oxygen then ensure you use it as regularly as required and as prescribed. There are workouts designed to help improve balance and stability which can help to minimize the risk. Adjust your home and activities to reduce the likelihood of a fall; not using stairs as often, moving objects to lower heights etc.
References: http://www.reuters.co
A stomach bug may offer hope for COPD patients
New studies have found that patients with COPD have a 3 times higher risk of having a certain bacteria within them. The bacteria heliobacter pylori, which is usually linked to the development of stomach ulcers may also be the trigger for lung disease.
Smoking is the main cause of COPD but research suggests that a big role may be played by the bacteria. It mainly colonizes the stomach but evidence suggests that is accumulates in the ears, nose, skin and even the eyes. It has previously been thought to be only involved in stomach ulcers and stomach cancers but recent studies have shown that the bacteria is also linked to other cancers, glaucoma, gall bladder, auto immune disease, iron-deficiency anaemia and other conditions of the eyes, ears, nose and throat.
One theory is that COPD patients may have a high level of this bacteria due to childhood infections that affect lung growth and make them more vulnerable to disease. Early eradication of heliobacter pylori in childhood may enable full lung development and reduce the risk of COPD in later life. The discovery could open the way for new preventative strategies.
- pylori stimulates the release of cytokines, which have an inflammatory effect on the body. When the infection and bacteria are eradicated then cytokine levels return to normal and inflammation decreases.
The findings may point to new ways of tackling COPD, because H. pylori can be detected with a breath test and treated with antibiotics. So it could mean that a simple course of antibiotics could kill off this bacteria, reduce the inflammation and reduce the severity of COPD symptoms immensely or if caught early then prevent COPD from developing.
References: http://www.dailymail.co.uk