Bronchiectasis is making a come-back
This lung disease from the 1800's has begun to reappear again, especially among the elderly. Historically cases were due to untreated chest infections where antibiotics weren't readily available and the poorer part of the community suffered with it more.
Research data from the NHS shows that of the 12000 patients admitted with Bronchiectasis in 2013-2014 most of them were over 60 years of age. Cases have doubled in the last decade among those aged 70 and over and now more than 1 in every 100 in this category will be affected.
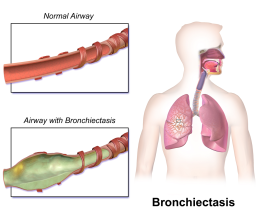
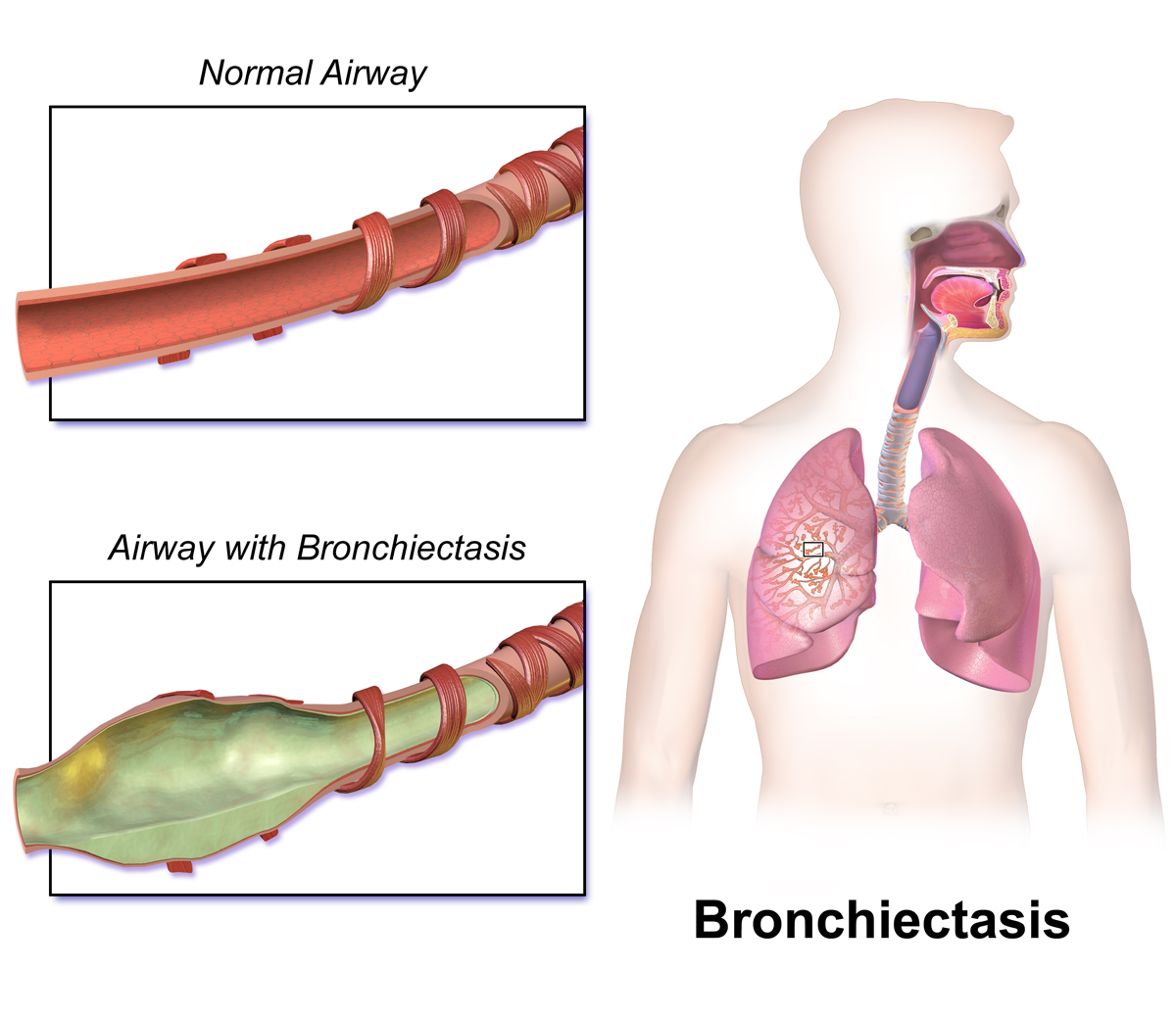
Bronchiectasis occurs when the airways of the lungs become abnormally widened, which results in chronic inflammation due to the inability to clear mucus secretions in the airway passages leading to a build-up of mucus. The excess mucus also harbours bacteria which can lead to worsening of the condition due to frequent infections. Symptoms typically include a chronic cough, shortness of breath, wheezing, fatigue, coughing up blood, and chest pain, along with worsening respiratory function. Inhaled antibiotics, bronchodilators, physical methods of dislodging mucus and oxygen therapy are all part of the treatment for this disease.
Experts agree that bronchiectasis may occur in people who suffered an infection in childhood such as pneumonia or whooping cough, which damage the lung. Underlying problems with the immune system and allergies are also thought to play a role. This is a main factor as to why the elderly are susceptible as with age comes a compromised immune system.
Bronchiectasis tends to occur as an after-effect of a chest infection such as whooping cough, tuberculosis, pneumonia or measles - particularly if the infection was not treated with antibiotics. Damage to the bronchi takes years to build up and symptoms don't tend to start until middle age, even if the original infection was years earlier.
'Antibiotics only really came in on a regular basis in the Sixties and Seventies,' says Professor Brown.'But we also see people who had antibiotics and despite that have bronchiectasis. Even if you treat it, the infection can still cause scarring, it's just less likely.'
The disease is incurable and although infections can be treated with antibiotics, there are concerns that the bacteria is becoming resistant to drugs.
Surprisingly more women are affected than men for no known reason other than for the fact that rheumatoid arthritis is a high risk factor for developing Bronchiectasis and this condition is more common in women. Also patients tend to be more affluent. 'We found the disease has had a resurgence in recent years, particularly among more well-off members of society,' says Jeremy Brown, a professor of respiratory infection at University College London. 'It could be partly down to improved diagnosis in these groups, but whatever the reason we need better treatment options.'
The study found that 42% of people with bronchiectasis also had asthma and 36% had chronic obstructive pulmonary disease (COPD). This is an important finding and can help with long-term management of these conditions. A study has found that COPD can be predictive of developing Bronchiectasis but that also this then makes the outcome for the COPD patient a lot graver.
The reasons for this disease increasing in certain groups is being investigated but it could be that it is running alongside the fact that diagnosis for other predictive diseases like COPD has improved in recent years but as to the reason why it is more prevalent in middle-class patients is unknown. With this rise of cases in recent years more research is now underway to improve treatment and to investigate the disease's coexistence with other diseases such as COPD.
References: http://home.bt.com and http://bronchiectasisnewstoday.com and http://www.dailymail.co.uk
Lupus and PH
PH or Pulmonary Hypertension is a disease that causes high blood pressure in the lungs due to narrowing in the pulmonary arteries by thickening of the vessel walls. It results in the heart having to work harder to pump the blood and the organ can become enlarged and weakened leading to heart failure. It can be caused by an underlying disease such as Lupus.

Lupus is a less common disease that many people haven't heard of. It is an autoimmune disease that occurs when the immune system attacks healthy tissues resulting in inflammation, swelling, pain and cell tissue damage. There are different types of Lupus but the most severe is systemic lupus erythematosus (SLE). Symptoms range from mild to severe, and many people will have long periods with few or no symptoms before experiencing a sudden flare-up, where their symptoms are particularly severe. Even mild cases can be distressing and have a considerable impact on a person’s quality of life. Lupus is a complicated condition and common symptoms are fatigue, joint pain and swelling and rashes, however the disease can cause systemic damage and can effect organs like the kidney, heart and lungs.
They are both very separate diseases and PH does not cause Lupus however Lupus can cause PH. Patients suffer from shortness of breath, fatigue and fluid retention; symptoms also seen in patients with PH. The development of lupus-associated PH is not completely understood and “it is not yet known, for example, whether lupus itself can directly cause PH, or whether lupus is simply a trigger for the development of [PH] in susceptible individuals,” the report explains.
It is more common in female patients to develop lupus and PH at a younger age (15-50 years) than those that traditionally develop PH alone. PH can worsen the symptoms of Lupus and it is important to diagnose it early. Individuals should be aware of swelling in the feet, ankles, legs and abdomen, difficulty in breathing, chest pain, light-headedness and fainting.
There is currently no cure for either PH or Lupus but there are treatments that can help to ease the symptoms. Medications to help with inflammation, swelling and to ease blood pressure as well as measures to deal with fluid balance and supplemental oxygen to help with breathlessness and oxygen levels in the blood. Oxygen therapy helps with both diseases simultaneously; by helping to reduce inflammation and increasing blood oxygen levels which helps in tissue repair to reducing breathlessness, easing the hypertension and decreasing blood pressure among many other benefits. If Lupus is in association with the PH then immuno-suppressive medications can sometimes be administered which help with the inflammation and irritation in the body however they can also cause damage in the blood vessels in the lungs which can be counterproductive. Lupus is still very much an unknown disease and with time and understanding of its processes there will hopefully be more effective treatments in the future that could ease Lupus symptoms as well as PH symptoms if the patient suffers with both conditions.
References: http://pulmonaryhypertensionnews.com and http://www.nhs.uk
COPD can cause brain changes that increases pain, fear and breathlessness
A recent study has revealed that patients with COPD exhibit a decrease of grey brain matter in certain areas of the brain that are responsible for processing breathlessness, fear and sensitivity to pain.

COPD is often accompanied by anxiety and depression as well as a fear of dyspnea and physical activity which contribute to the disabling effect of the disease and fuels the downward spiral of avoidance of physical activity and subsequent reduction in health and quality of life.
Unfortunately, little is known about underlying brain processes in patients with COPD and the relationship with disease duration and disease-specific fears but this recent study is starting to help to change that. The results revealed that patients with COPD showed a decrease in grey brain matter volume in specific areas of the brain, namely the cingulate cortex, hippocampus and amygdala. The levels of degeneration were also directly linked to length of disease, so the longer the patient has had the disease the greater the decrease in brain matter. The individuals showed a greater fear of breathlessness and fear of physical activity where there was also a reduction in brain matter in these areas and again was directly linked to length of time having had been diagnosed. Proving that over time COPD patients will suffer and decrease in brain matter in specific areas of the brain which affects their ability to process fear and as a result become increasingly breathless and more fearful of physical activity.
This increasing fear has a detrimental affect on the course of the disease and on quality of life. Exercise and keeping active is extremely important for COPD patients to ensure their condition doesn't deteriorate. Therefore “targeting disease-specific fears in patients with COPD might not only improve outcomes of clinical interventions such as pulmonary rehabilitation, but also reverse structural brain changes in these patients,” concluded the research team.
This study helps to prove just how complicated the disease is; how it also affects the brain and its impact upon your mental and emotional state. Hopefully they'll discover a treatment to combat these effects upon the structures of the brain but until then it is even more important to ensure you take medication and supplemental oxygen to keep you as alert and as medically fit as possible so you are able to keep active and enjoy your life. Oxygen has a great positive effect on your brain and on your emotional and mental state and is a great treatment at the moment to combat these side effects in the brain.
References: http://lungdiseasenews.com
CPAP can help ease many symptoms
Fibromyalgia is a condition where a person will experience all-over body pain due to their being unable to sleep because of the body pain, which is a vicious cycle. It is linked to sleep disorders such as sleep apnea, insomnia and restless leg syndrome.

Restless leg syndrome (RLS) is a condition that causes a person to feel an overwhelming urge to move their legs when laying down and they experience tingling, aching and itching sensations. Restless leg syndrome is classified as a neurological disorder that can impair a person’s ability to fall asleep.
Fibromyalgia and sleep disorders go hand in hand as pain causes the individual to not be able to sleep and the lack of sleep leads to more pain. If a person manages to get some proper sleep then the symptoms start to ease.
A study revealed that those who suffer from obstructive sleep apnea may also have Fibromyalgia and they also found that using continuous positive airway pressure (CPAP) was an effective treatment for both conditions. A CPAP device is a machine that supplies oxygen continuously via a face mask while you sleep to prevent any obstructed breathing.
Another study found that patients with Fibromyalgia have a high risk of developing or already having restless leg syndrome by ten fold. Sleep disruption can cause the development of RLS but also having RLS can lead to developing Fibromyalgia.
Due to the interlinking nature of all these conditions, then by treating one you can ease or prevent other conditions from developing. CPAP can treat sleep apnea and aid in a patient getting a proper night's sleep which will in turn ease Fibromyalgia symptoms and can in turn also ease or prevent RLS. Also treating the Fibromyalgia or RLS can reduce the pain and aid in getting a proper night's sleep.
CPAP machines have a mask that fits over the nose and mouth that provides constant airflow, keeping the airway open and the sleeper breathing throughout the night. CPAP machines also track breathing changes and that data is used by health care professionals to adjust, as needed, the air pressure as well as possibly add additional treatments or medications for maximum effectiveness. Because some of the most effective CPAP machines are rather robust and cumbersome when it comes to traveling many leave their machines at home. A travel CPAP machine is a smaller, more compact version of a traditional CPAP. They don't include a humidifier but most people are willing to give this up for the convenience. Many of the newer travel CPAP machines also have the benefit of being able to monitor and record sleep data.
Whether you have a sleep condition that worsens your Fibromyalgia or your Fibromyalgia wrecks your sleep, sleep can improve Fibromyalgia Here are some tips to help those with Fibromyalgia improve their sleep.
- Don’t oversleep – only sleep the length of time you need to feel refreshed.
- Keep a sleep diary so you can review what woke you and other sleep factors.
- Stick to a sleep schedule.
- Use relaxation therapies – this may also improve RLS.
- Exercise regularly.
- Create a proper sleeping environment – cool temperature and a dark room.
- Avoid long daytime naps.
- Don’t go to sleep hungry or on a very-full stomach.
- Avoid caffeine prior to bed.
References: http://www.belmarrahealth.com and http://www.huffingtonpost.com
Dubai
Dubai has a misunderstood reputation of being unsafe, all about the 'bling' and the rich, being soul-less and being intolerable to non-Islamist visitors. However this is a misconception and if you scratch the glittery surface you'll find a culture, open-minded and warm city. More than a million Brits have holidays in Dubai each year, which is more than the total number of people who go skiing across the world. Dubai has risen from the sand in just 25 years and boats the biggest, tallest, fastest and most expensive of everything.

Dubai does enjoy having the biggest and best of everything and holds many records from the tallest building on Earth to the world's biggest shopping centre.
If you want to remain in a resort then The Palm is the place to be; a man-made peninsular in the shape of a palm tree by a man-made lagoon with a spectacular hotel resort-cum-fantasy castle. It allows you to hop in a fish tank and be surrounded with 60,00 fish, hammerhead sharks and stingrays. There's snorkel sessions at the aquarium among the sharks and stingrays which you can also feed. On the 42 acre site there are 2 lake-sized swimming pools, a water park and a beach. 23 restaurants offers you a huge range of places to eat offering a huge range of cuisines so you can eat in a different place each day.
Nearby to the resort there are other beaches and an array of restaurants as well as the Dubai Mall which is the biggest in the world and is larger than 50 football pitches. It is attached to the worlds tallest building the Burj Khalifa tower with an observation deck on the 124th floor. There is the Dubai aquarium and underwater zoo with amazing creatures from all over the world and an Olympic-sized ice rink and 22 screen cinema. Most hotels and public buildings also smell amazing due to perfumed air-con which just adds to the experience.
Its difficult to remember that most of Dubai is actually covered in sand but an evening desert safari will quickly remind you of this fact and after a camel ride and meal by an open fire you can spend the night in the desert under the stars.
Dubai offers luxury and glitz and glamour in every aspect you can think of and you definitely find ways to pamper yourself while you are there. On the flip-side there is also the tradition, culture and history of the region with traditional dancers and entertainment as well as museums to visit. Dubai is proud to be tolerant of all religions and races and has a variety of churches and temples as well as openly celebrating other religious holidays such as Christmas and Easter with decorations proudly put up and Christmas tunes playing in the shops. Female expats remark upon how safe they feel living here and the city is practically crime and violence free. It definitely has a lot more to offer than just being an adult Disneyland and is enjoyable for all ages. The temperatures do climb however and therefore winter-time is the preferable time of year to visit.
Even though Dubai is a bit further to travel to, it is still a viable travel destination if you have medical requirements, as companies such as Oxygen Worldwide now provide medical oxygen to Dubai as well as to the majority of countries around the world. It is mostly flat and with air-con in most buildings you can keep cool in the heat and with portable concentrators you can move around and explore and enjoy all of what Dubai has to offer.
References: http://www.dailymail.co.uk and www.mirror.co.uk and http://www.telegraph.co.uk
'ORGAN-ON-A-CHIP' technology could be the future
A research team at the Wyss Institute for Biologically Inspired Engineering at Harvard University have used their new 'organ-on-a-chip' technology to develop a model of the human airway so that diseases such as COPD can be studied outside of the human body to allow researchers to gain new insights into the disease mechanisms, identify biomarkers and test new drugs.
Diseases such as COPD and asthma are inflammatory reactions in the lungs whether to smoking, inhaled particles or bacterial/viral infections. It is already known that many of the disease processes occur in the alveoli however much less is known about how inflammation starts off these reactions and why these processes react in the way that they do. For example the reason why the body recruits white blood cells and the build-up of mucus, both of which compromises the patient's lungs or the cause and reasoning behind exacerbations.
A new microfluidic model of the lung has been created of the lung's small airways made with chips lined with cells from both normal donors and diseased patients. This model is like looking inside an actual patient and “recapitulates critical features of asthma and COPD with unprecedented fidelity and detail” explains Donald Ingber. Now with this micro-engineered human lung small airway lung inflammatory diseases over several weeks can be studied in order to gain better insight into disease mechanisms, as well as screen for new therapeutic drugs.
This device closely mimics the 3D cellular architecture of an actual human small airway and contains fully matured human small airway epithelium with different cell types and channels containing all the components that you have in your lungs including white blood cells and nutrients. The device can keep itself 'alive' for a few weeks before starting to deteriorate. Inflammatory situations such as asthma and COPD can be simulated by adding an asthma-inducing immune factor or by setting up the system with lung epithelial cells from a COPD patient and then researchers can observe the different ways that the airways react in different situations. In both cases, the team was not only able to observe highly disease- and cell type-specific changes but could also exacerbate them with agents simulating viral or bacterial infection.
Demand for such a device is high due to the fact that the inflammatory response is so complex and internalised that it cannot be adequately studied in humans or animals and there are no known drugs that can stop and start the inflammation processes so that you could potentially get a snap-shot of what was going on.
This new organ-on-a-chip technology has provided researchers with a window on a molecular scale to be able to observe the activities of living human tissue and allows them to break down the processes and interactions of specific cell types and immune system components so as to understand why the diseases progress in the way they do and ideas on how this could be prevented based on the interactions between the lung tissue and the immune system, whether this be by manipulating the immune system response or by developing new drugs to counteract the effects.
"This novel ability to build small airway chips with cells from individual patients with diseases like COPD positions us and others now to investigate the effects of genetic variability, specific immune cell populations, pharmaceutical candidates and even pandemic viruses in an entirely new and more personalized way; one that will hopefully increase the likelihood of success of future therapeutics," said Ingber.
References: http://medicalxpress.com
How your cough can impact on your quality of life
The characteristic symptoms of COPD include a chronic and progressive cough and sputum production that can be variable from day to day; it may start off intermittently but towards the end will be frequent throughout the day.

The cough itself is an important defence mechanism that helps to clear foreign bodies and excess mucus from the lungs to allow better breathing. However a chronic cough has been found to be associated with detrimental psychological and physical effects on the patient's life.
Depression, muscle strain and fatigue, sleep deprivation, incontinence and vomiting are all directly associated with coughing. Other related symptoms are rib fractures, fatigue, embarrassment, unconsciousness, difficult conversations on the phone, hoarse sound, unable to stand close to the their relatives due to their cough, and an inability to work in school or elsewhere.
In this new study it has been shown that a lower cough-specific quality of life is associated with a lessened ability to carry out daily activities due to its negative effect on fatigue and lower abdominal muscle endurance, and higher depression levels are also usually observed in patients with COPD.
When coughing the contraction of abdominal muscles is required. However with a chronic cough this can lead to a decline in the endurance of these muscles due to repeated overuse and resulting in them working ineffectively and not being able to help aid the cough or mucus clearance.
In a study of COPD patients with chronic coughs 33% were identified as anxious while 16% experienced depression and approximately 48% of all coughers had moderate or high trait anxiety. Also in general patients were at a higher risk of suffering from phobic anxiety, obsessional tendencies and depression showing that this group of individuals suffered from an emotional and psychological impact on their lives from their chronic cough.
53% of the group attended a speciality centre to help treat their chronic cough and depressive symptoms and there was a statistical improvement in both cough severity and depression scores after three months. This reinforces the fact that quality of life and chronic cough are linked but also that there is treatment to help improve both.
If cough is an important part of COPD and contributes to deterioration in quality of life, the symptom should be controlled and see your doctor who can help to ease your cough which in turn will hopefully improve your quality of life whether physically, psychologically or both.
Ensuring that you follow your doctor's advice regarding medications and oxygen therapy regime, exercising and eating correctly will help to ensure that you are easing the COPD symptoms as much as possible and therefore also the cough. If you find you are coughing more and gasping for breath maybe your medical oxygen requirements need altering; whether it be an increased flow rate or different machinery to fit your lifestyle. Ask your doctor straight away as anything that you can do to ease the coughing and breathlessness will not only instantly improve your medical condition but will indirectly improve your general quality of life.
References: www.dovepress.com
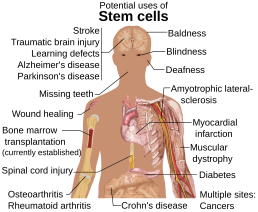
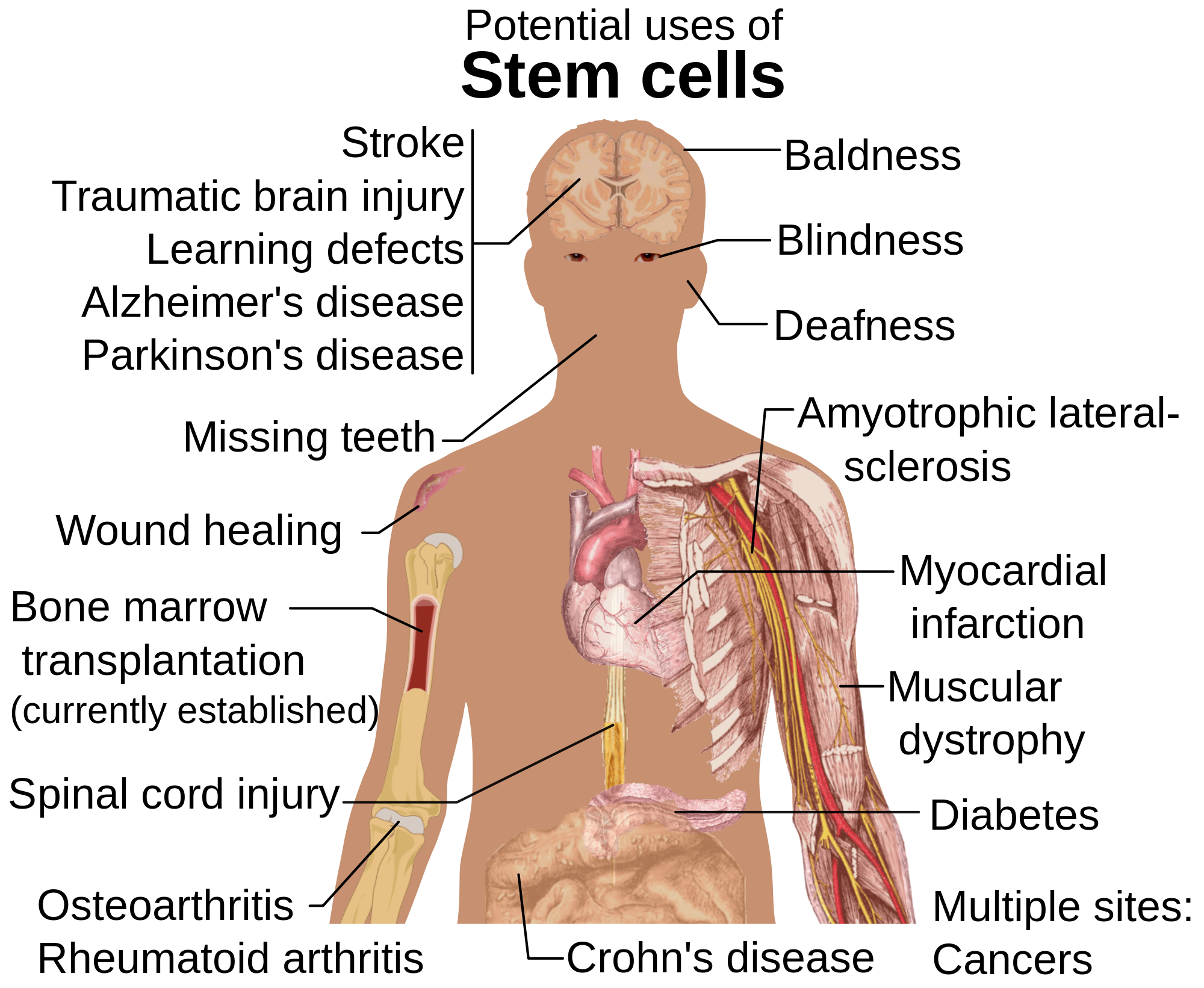
Stem cells and nanoparticles could be the future treatment for lung disease
Malaysian scientists are joining forces with Harvard University experts to help in seeking a safe, more effective way of tackling lung problems including chronic obstructive pulmonary disease (COPD), the progressive, irreversible obstruction of airways causing almost 1 in 10 deaths today and to revolutionize the treatment of lung diseases through the delivery of 'nanomedicine.'
Treatment of COPD and lung cancer commonly involves chemotherapeutics and corticosteroids which are misted into a fine spray and inhaled, enabling direct delivery to the lungs and a quick and effective medicinal effect. However, because the particles produced by today's inhalers are large, most of the medicine is deposited in the upper respiratory tract and does not reach down to lower parts of the airways and lungs.
The Harvard team is working on "smart" nanoparticles, which are tiny particles that deliver the appropriate levels of a medication to the deepest, tiniest sacs of the lung and ensures an even distribution, through the use of magnetic fields.
Malaysia's role is to help ensure the safety and improve the effectiveness of nanomedicine and in assessing how nanomedicine particles behave in the body, what attaches to them to form a coating, where the drug accumulates and how it interacts with different cells.
Inhaled nanomedicine holds the promise of helping doctors prevent and treat such problems in future, reaching the target area more swiftly than if administered orally or even intravenously. This is particularly true for COPD and lung cancer, says Dr. Brain. “Experiments have demonstrated that a drug dose administered directly to the respiratory tract achieves much higher local drug concentrations at the target site.”
"Nanotechnology is making a significant impact on health care by delivering improvements in disease diagnosis and monitoring, as well as enabling new approaches to regenerative medicine and drug delivery," says Prof. Zakri Abdul Hamid, Science Advisor to the Prime Minister of Malaysia.
Lung regeneration is another key focal point as scientists have found that regardless of their stage in life, lung cells are able to regenerate themselves in order to repair missing or damaged tissue. The team behind the discovery hopes that they will one day be able to replicate this natural behavior in order to help repair tissue damage in patients with conditions such as COPD.
There are two main types of lung cells: type 1 cells, where oxygen and carbon dioxide are exchanged during breathing and type 2, which secrete surfactants, a type of lubricant essential to the breathing process. Type 2 cells have been previously observed to regenerate into type 1 cells in the presence of cell damage, but a team of scientists from the University of Pennsylvania School of Medicine and Duke University have shown that the opposite also occurs.
"We saw new cells growing back into these new areas of the lung. It's as if the lung knows it has to grow back and can call into action some type 1 cells to help in that process," explained cardiologist Rajan Jain and the observation suggests that there is much more flexibility in the pulmonary system than previously thought.
Understanding how and why these mature cells are regenerating into different types of lung tissue may be the key to treating certain types of lung damage caused by conditions such as chronic obstructive pulmonary disease. Although patients may somewhat control the condition, there is currently no cure. The ability to regrow damaged lung tissue on demand, then, could completely change treatment options and possibly offer a cure for COPD patients.
References: www.news-medical.net and www.medicaldaily
You soon could wear a blood oxygen sensor like a plaster
For many patients such as those with COPD it is important for your health to be able to constantly monitor your blood oxygen levels in order to avoid exacerbations and worsening health and breathing problems. There are many pulse oximeter devices already out there but many are cumbersome or difficult to use. These rely on LEDs that shoot infrared light and red light through a part of the body with a sensor waiting on the other side to receive the light that remains and detects how much has passed through. Oxygen-rich blood will absorb much more infrared light and low-oxygen blood will absorb more of the red light.

Scientists at the University of California have a developed a much more simplified, easy to use and light weight device by developing a thin film-like sensor that can be worn around the finger much like a plaster. Instead of using infrared and red light this new device uses red and green light. These red and green LEDS are organically made and integrated onto a flexible piece of plastic.
Due to the organic components this electronic device is flexible and can easily conform to the body. It also means that the parts are cheaper to make, meaning that they can be thrown away after each use rather than having to disinfect the device each time. It is lightweight, more inconspicuous, cheap and disposable. The researchers tested the prototype alongside conventional pulse oximeters and found the readings to be equally as accurate.
Another device which is only the size of a post-it note is the Moxy-monitor, which has been designed to allow the user to monitor their body performance during workouts. It is a small black box worn against the skin that tracks blood oxygen levels in your muscles and it can display the data along with other fitness data in real time in third party devices and apps. It uses LEDS and light detectors to transmit near-infrared light though the skin and into the muscle tissue and back out again and extracts oxygen level readings from the results.
Although the device is geared more towards athletes, it is also beneficial for anyone with a medical condition such as COPD who want to exercise to help improve their condition but who need to monitor their oxygen levels closely to make sure they do not over do it and end up collapsing out of breath. The developers say that it is durable, even for rugby players and can even be used underwater. Its charge lasts for 3 hours and it transmits its data via a radio antenna or data can be retrieved via a USB port if the device has been out of signal or underwater.
There are other devices that have been developed such as a smart sock that monitors a baby's vital signs and iPhone compatible oximeters. The future however is set to explode under the term 'wearable.' Much more than smart watches and fitness bands, the market is set to be filled with garments laden with sensors sewn into them which can track and monitor our every move.
These garments will at first be aimed at runners and sports professionals who want to track their performance, but will quickly spread to help anyone who wants to keep tabs on their health. Sensors sewn into clothing will scan for heart conditions, Smart socks will help those recovering from injury to restore their balance and alert family members when an elderly relative suffers a fall. The clothing manufacturers and fashion world are keen to weave these devices into their clothes so that users can be fashion conscious and advertise sponsors and brands as they move around .
Looking further ahead 'wearables' will become medical devices more than fitness trackers. When the data from them is accurate enough to be used to monitor someone's heart over a period of time then their doctor could tell when the data is indicating a heart condition.
People in the industry believe that this will be a vast market and incredibly popular and that it will make such sensors cheap enough to sew into a whole range of clothes, and for them to be durable enough to be washed. They also forecast that these sensors could also be offered to users outside of retail such as with health insurance, gym membership and with diet plans.
References: http://www.gizmag.com and http://www.ibtimes.co.uk
Computers could help treat us 24/7
Normally your GP may see you for a few minutes a few times a year and take a handful of test results. What if a computer system was constantly monitoring you 24/7 and could compare your results with readings from thousands of other patients worldwide and use the knowledge from clinical guidelines and studies to treat you?

In 2016 this idea is closer to becoming a reality. A machine in California has been designed by Sentrian, an early-stage machine learning and biosensor analytics company for remote patient management to be able to do this and is currently being trialed on patients. “We are trying to build a system that will enable us to listen to the lives and bodies of patients all the time, so we can make better, earlier and more personalised decisions."
Currently one or two wireless 'biosensors' can collect simple data such as body temperature and heart rate as well as more complex information like oxygen saturation and potassium levels. If a patient could constantly wear several sensors at a time then the amount of data produced would be enormous.
Collecting all of this data and using learning algorithms to detect subtle patterns on chronic conditions such as heart disease and COPD can allow the machine to be able to detect early warning signs of an exacerbation or an attack and notify the doctor and patient when needed to warn them and allow more accurate treatment.
Many patients with COPD and similar chronic conditions will have symptoms a few days before an attack occurs but not feel ill until nearer the time. The computer could detect early signs of an upcoming attack and warn the doctor and patient so that medications could be altered, oxygen levels adjusted or warn the patient to eat or sleep more etc. It is currently being tested in the US and UK and early evidence has shown that the computer can spot early signs of a congestive heart failure exacerbations up to 10 days in advance. Early research is showing that even small things like heart rate change, sleep duration and body temperature may be indicators of an impending crisis and the system can even predict when someone may suffer a fall well in advance.
However the question being discussed is whether we should hand over all decision making to a computer when it comes to health-care? The profession itself is non-trusting of the results and of a computer being in control but Sentrian have suggested having joint control with humans. That doctors are notified of results and warning indicators and can use their judgment accordingly. The computer system would also be continually learning to know exactly which rules and interventions work best for which patients, and if a false alarm occurs the doctor can report this and the more feedback the system gets, the more it can learn and adapt.
Normally the human brain can remember the last 30 patients but the computer would be able to remember more than 30,000. Machine learning is also a lot faster than human learning. With the medical advances and research of the last 100 years medical knowledge has grown beyond belief and is becoming more difficult for the human brain to be able to intake and even during the course of a GP's life medicine is constantly progressing and it is difficult for a GP to keep up-to-date. On average it can now take 17 years for new evidence-based findings to find their way to the GP and be clinically used.
What if a doctor was able to bring up every single case study and worldwide guidelines on a particular disorder to the forefront of their minds and instantaneously have all the possible data they need? The computer system can do this and therefore will you not be treating the patient with the most up-to-date knowledge possible? It could read all textbooks, medical databases of journals and literature, thousands of patients records and be subject to 1000's of hours of teaching sessions from clinicians. Things that can take scientists 30 years to uncover may take the computer only a month, especially when it comes to research.
It could assist your GP by analyzing a patient's medical record in conjunction with all of it's acquired knowledge and suggest potential treatment recommendations. It could also match patients to clinical trials which usually takes hours of a human's time to trawl through patient's notes to see if they match the criteria for a trial and eliminates human error.
In theory by wearing a few sensors a computer system can monitor and record your readings, recognize subtle patterns and differences in your results, use data collected from around the world and if there are indicators for different treatments, a warning sign of an attack or deterioration of your condition then it can alert your doctor and you. It may just require a slight alteration in your medication dosage or oxygen saturation levels or ask that you eat, exercise or sleep more; things that the patient can do themselves or it may require intervention from the GP or hospital.
“Sentrian's system is currently undergoing several randomised controlled trials, which means that the data of thousands of patients will be added to the platform. While we wait on clinical evidence, it is just a matter of time before this sort of artificial intelligence becomes a regular occurrence in the doctor's office.”
References: http://www.wired.co.uk