Exercise table could help alleviate COPD symptoms
A team of researchers in America have developed and are currently testing out a table that may be able to help patients that suffer from the effects of COPD.

The team consists of people from all disciplines that have come together to pool their knowledge of COPD and patient's pulmonary care and treatment to help these patients to improve their breathing.
The table is based on a gravity-powered approach to improve ventilation as well as helping to clear mucus. The table appears stable but in fact rocks forward and backwards with weight. The person on the exercise table lifts and pulls a bar while rocking the table forward
As the person pushes away the table then rocks backward resulting in the person's feet being higher than their head. This movement forces air out of the lungs, which is normally difficult for a COPD patient to do and therefore reduces the difficulty of breathing for the patient. This approach also uses gravity to help the tiny hairs in the lungs to move the mucus along the trachea as well as the gravity also helping to move the lymphatic fluid out of the lungs. The movement of the abdominal viscera also moves the diaphragm which also reduces the effort of breathing.
The table not only aids the lungs and breathing but also benefits the rest of the body. The gravity effect on the body results in the drainage of lymphatic fluid from the arms and legs, improving circulation and reducing swelling.
One of the founders of the company is himself a COPD sufferer and says that the table has alleviated his symptoms greatly but the table is currently being vigorously tested in trials.
References: http://copdnewstoday.com
Using opioids worsens your COPD
COPD patients are often prescribed opioids such as codeine, oxycodone and morphine to provide relief from common symptoms such as muscoskeletal pain, insomnia and respiratory issues. However it has been shown by researchers in Toronto, Canada that opioids can induce additional respiratory side effects and that new opioid users have 5 times a greater risk of death compared to non-opioid users. These results raise serious safety concerns about the use of opioids for older adults with COPD.
“This is a population that has a chronic lung disease, with symptoms that can sometimes be challenging to manage,” said Dr. Nicholas Vozoris, lead author of the study. “This class of drugs may offer some relief; however, there is also evidence suggesting that opioids can adversely affect breathing and lung health in people who already have chronically compromised lungs.”
Previous studies reported that opioids were safe for patients with advanced COPD but the results were not reliable due to study limitations.
In this new study over 130,000 patient records were examined from multiple healthcare databases to try to ensure the results were more generally applicable and reliable.
“Previous research has shown about three-quarters of older adults with COPD have been prescribed opioids, which is an incredibly high rate of new use in a population that is potentially more sensitive to narcotics,” Vozoris said. “Our new findings show there are not only increased risks for respiratory-related death associated with new opioid use, but also increased risk of visits to emergency rooms, hospitalizations and needing antibiotics or steroid pills.”
The team found that those who used opioids had an increased risk of 14% or ending up in the emergency department and nearly 3 times the risk of COPD or pneumonia-related mortality. They even have an overall mortality risk of 76% compared to non-opioid users. Opioids were however found to decrease the risk of respiratory exacerbations by 12%.
The higher risks were found in patients using stronger or higher dosage opioids however many risks were unaffected by dosage if you were a new user.
Opioids can impact COPD patients in several ways such as respiratory depression, reduced mucous clearance from cough suppression, and immunosuppressive effect.
To lower the risks of adverse events doctors may prescribe less potent or lower dosage opioids but the results of the current study showed increased risk of complications and even death regardless of dose amount among new opioid users. Vosoriz said the finding is important because lower doses were long considered safe.
“Sometimes patients are looking for a quick fix for chronic pain or breathing issues and physicians may believe opioids can offer them some relief,” he added. “The trade-off becomes explaining that there are risks to patients and making sure they understand that potentially alleviating their symptoms could come at a higher cost to their health.”
An individual multi-disciplinary approach is better as a treatment plan rather than just prescribing opioids. Making use of pulmonary rehabilitation, supplemental oxygen therapy, exercise and lifestyle changes in conjunction with medication is best way forward for COPD patients.
References: http://copdnewstoday.com and http://lungdiseasenews.com
Non-pharmacological Treatments for COPD
Despite there being excellent medications for COPD patients, such as bronchodilators which are continually improving in both potency and in delivery there is still a huge proportion of the COPD patient population who continue to experience deterioration in their symptoms and poor quality of life. There are however many non-pharmalogical treatments that can provide huge relief for many patients. They may work alongside your pharmalogical treatment or you may decide that they are better used instead of, but always consult with your doctor.
Smoking cessation is the most important of these. It has been shown and still being proved in continuous research how cigarette smoke harms not just your lungs but also the rest of your body. It the primary cause of COPD and the chemicals have been shown to affect your cells right down to its DNA and causes abnormalities, inflammation and permanent damage which greatly worsens your symptoms and respiratory ability. There are lots of different ways you can be aided in stopping, with patches, gum and electronic cigarettes. Its always best to support your method with counselling or support groups.
Telemedicine allows patients with COPD to connect electronically with a specialized care consultant. Telemedicine can be used to collect information from the patient and track his or her progress on a daily basis, if necessary. It has been used to alert the medical team to the early onset of acute exacerbation of COPD thereby avoiding emergency department visits and hospital admissions. However, more evidence is needed as some studies state that "telemonitoring for COPD is not yet proven and further work is required." There are many devices already out in the market which are easy to use and allows the user to feel more in control and to monitor their respiratory vitals on a daily basis and adjust their regime quickly when alerted to avoid unnecessary attacks and deterioration.
Pulmonary rehabilitation is important in order to sustain your mobility and quality of life. It aims to counteract the loss of skeletal muscle that is common in COPD and to improve exercise tolerance. There are a variety of methods including exercise training, nutritional supplementation, and psychosocial support. Although it is not yet proven to have direct links to increased survival or lung function, there have been improvements in health-related quality of life, dyspnea, and exercise tolerance. There has also been a tendency for any accumulated improvements to deteriorate with time unless the methods are continued.
Long-term oxygen therapy is also an option for some patients with COPD. Short-term use of oxygen during exercise or strenuous activities in patients with any degree of hypoxemia has long been known to improve dyspnea and increase exercise tolerance, although is not proven to extend survival. For patients who are chronically hypoxemic long-term oxygen therapy where the patient uses it constantly through the day, not only improves exercise performance and quality of life but also improves survival rates. There are many different devices depending upon your lifestyle and requirements and can be obtained via the NHS or from private companies. They are much more compact, lightweight, discrete and portable than ever and still allows the patient to move around easily both in their home and outdoors so as to allow the patient to have a significantly increased quality of life and eliviate respiratory symptoms.
Noninvasive positive pressure ventilation (NIV) has been effective when treating COPD patients that suffer from acute exacerbations. Gas exchange and respiratory abilityes are improved, resulting in decreases in intubation rates, shortening hospitalizations, and improving mortality. However, its long-term role in managing COPD has not been demonstrated and its unclear as to whether nocturnal NIV will signoificantly improve lung function, gas exchange, or sleep efficiency.
Patients with severe emphysema typically have bullae. These are growing air spaces that occupy space within the thorax but do not provide much gas exchange. They are more likely to impair the function of less diseased lungs by occupying dead space within the thorax and contributing to air trapping and ventilation/perfusion problems. The aim of surgical lung volume reduction is to remove nonfunctional lung and thus improve lung physiology and symptoms. A large study showed that this treatment is only truely beneficial to patients with predominantly upper lobe disease and low prior exercise tolerance. Other subjects tended to have higher mortality. The procedure is rarely performed today, but there are attempts to achieve a similar outcome, by less invasive methods. These employ the placement of one-way valves in the lung airways that allow gas to leave bullae but not return. The valves are placed bronchoscopically into the lungs. In general, some improvement in lung function, less dyspnea, and improvements in exercise capacity have been obtained, but there has usually been an increase in adverse effects, including acute exacerbations of COPD and pneumothorax, sometimes requiring removal of the valve(s). Lung coils are another method proven to be very succesful. Doctors insert special flexible scopes through the patient’s mouth to place metal coils into the damaged tissue of the patient’s lung. The coils return elasticity to the diseased tissue, allowing the lungs to work in a more normal way. Other experimental lung procedures with the same aim have attempted to collapse the most emphysematous lung regions by closing the airways to those regions by other means, but development of these methods is incomplete.
Lung transplantation has been an option for patients with severe COPD since 2000, with 50% survival being in the region of 5 years and steadily improving. It should be considered only in patients with end-stage COPD, only when all other therapies have been tried and failed to provide relief. Primary graft failure, chronic rejection, and infection are common problems, however, there can be successes where lung function and quality of life can markedly improve, and outcomes are improving with time.
References: www.medscape.com
Cigarette smoke affects your DNA
A recent study proposed the idea that damage to our DNA at the telomeres contributes to lung ageing, continuing damage and worsening COPD symptoms. Also that cigarette smoke increases and encourages such damage to the telomeres.

Telomeres are specialized structures at the ends of chromosomes within our DNA that protect it from deterioration and prevent fusing with nearby chromosomes. COPD has long been associated with accelerated lung aging and abnormal cell division. Telomeres shorten with each cell division, therefore the more the cell divides the less protection the DNA strands have.
In a newer study they investigated telomere dysfunction in lung airway cells from patients with COPD using lung aging mouse models exposed to cigarette smoke. They found that there was no difference in telomere length between control patients and COPD patients, which contradicts the previous study although they say that this could be due to a small sample size and will need to be repeated with a larger amount of samples.
With age they observed an increase in telomere dysfunction and that this was also increased with exposure to cigarette smoke. They found that the cigarette smoke accelerated the telomere dysfunction by increasing levels of reactive oxygen species (free radicals) and aided in the secretion of inflammatory cytokines.
As a result, the team highlighted that their findings suggest that telomeres are particularly susceptible to damage triggered by cigarette smoke, and that this may lead to an accelerated decline of lung function in both aging and COPD patients. So whether you have COPD or have normal respiratory health, exposure to cigarette smoke will trigger telomere dysfunction, affecting the DNA within the cells and causing damage to the cells in your lungs. And thereby reducing respiratory function in the elderly and worsening symptoms in COPD patients. This study suggests that the elderly and patients suffering from respiratory illness should not only stop smoking but also not be around other smokers in order to preserve their respiratory health.
References: http://copdnewstoday.com
Possible cure for PAM and other rare lung diseases?
Pulmonary Alveolar Microlithiasis (PAM) is a rare lung disorder where small stones form and accumulate in the air sacs of the lung. These stones cause inflammation, scarring of lung tissue and reduced respiratory ability resulting in the patient requiring supplemental oxygen.
New research from a team at the University of Cincinnati has uncovered and identified key bio-markers and a potential new therapeutic approach that could be the key in treating this rare lung disease.
A few years ago a team discovered that DNA mutations in the gene SLC34A2 caused a loss of a cellular pump which would normally remove phosphate from the air spaces in the lungs. As a result calcium and phosphate levels rise in the alveolar sacs and cause the formation of stones or microliths that invoke inflammation. Patients find that by middle-age this chronic inflammation has caused scarring and damage to the lungs and experience respiratory failure.
The team collected samples from people all over the world with help from the RDCRN programme who's goals are to advance medical research on rare diseases by providing support for clinical studies and to facilitate collaboration and data sharing. This enables scientists from multiple disciplines at hundreds of clinical sites around the world to work together to help study more than 200 rare diseases.
They found that those with mutations in this specific gene also had elevated levels of certain serum markers. Certain cytokines and surfactant proteins were raised in line with the presence of stones in the lung, suggesting that by testing and monitoring these levels it could be a useful tool in following the disease progression and treatment responses in patients.
They also discovered that the stones dissolved easily in EDTA, a molecule used in many detergents as it binds to calcium. "Washing the lungs with an EDTA-containing solution reduced the burden of stones in air spaces," says Dr McCormack. "This finding could translate into a therapy for humans if toxicity studies demonstrate that the approach is safe."
A low-phosphate diet was found to prevent stone development and to even reverse lung calcification. However low phosphate levels can cause other medical problems and this approach will need to be tested in clinical trials first. Although another strategy is to utilise gene therapy and to insert a gene for a working phosphate pump back into the cells using viral vectors.
"This study demonstrates how discovering the causes of these rare lung diseases not only can inform us how the lung normally functions, but can also lead us to potential therapeutic interventions for these rare and often lethal lung diseases," says James Kiley, PhD, Director of the Division of Lung Diseases at NHLBI.
McCormack says rare disease research can reveal surprising insights into the fundamental biology of the lung. "Studies of the PAM.. model have already revealed a potential role for phosphate in the regulation of surfactant balance in the lung and have attracted the interest of cystic fibrosis scientists interested in exploring the possible interaction between [the phosphate pump] and the defective chloride channel in that disease," explains McCormack.
Although human trials are a few years way, UC's research offers some hope to patients who suffer from this rare disease. Kathleen Falco, 65 from Riverhead in America shares a similar story with other patients. She was misdiagnosed with Sarcoidosis in 1977 until 2000 when they diagnosed PAM. It started to take its toll in her 40's and a few years ago her symptoms intensified and she has shortness of breath, reduced mobility and dependency on supplemental oxygen. She cant walk, take part in outdoor activities, has lost weight and finds it hard to breathe when its hot or cold. She felt isolated, with little information and no support network or forums and eventually sort out help through the internet and was put into contact with Dr McCormack. She's hoping that the trials will be a success and that she may be able to live out her retirement years being able to breathe a bit easier and enjoy a much improved quality of life.
References: http://medicalxpress.com and https://www.sciencedaily.com
Asthma can reduce your productivity
A new survey has shown that 75% of people who suffer with asthma blame their illness for a significant reduction in productivity at work and asthma patients on average miss 3 hours of work a week due to their illness. The survey also showed how patients are also feeling that they have a lack of productivity when it comes to household chores and daily activities as well as at work.
All 1,598 patients surveyed were taking their prescribed medications and were from various countries. 74% reported issues around productivity at work and also 3 hours of work missed a week. 9% reported a complete inability to work and 67% reported sleep disturbances.
The survey was conducted by the Think.Act.Breathe campaign who help asthma patients identify personal risk and improve immediate and long-term risk of asthma exacerbations.
Dr. Kevin Gruffydd-Jones, lead author of the report said the findings illustrate how asthma can impact a patient’s economic burden, even while on medication.
“People with asthma often accept their symptoms and the impact they have on their daily lives. It is important that people with asthma talk to their doctor about how their asthma is affecting them at work, their sleep and daily life, and to discuss what more could be done to help them feel better and live life to the full.”
Asthma may cause physical and mental affects as well as the obvious physical ones and can have an impact on your whole life. Only 13% reported no impact on their work but 23% reported feeling tired and weak at work as well as 18% feeling mentally strained. 51% also stated that their symptoms had a negative impact upon their ability to complete daily chores outside of work.
“Asthma affects millions of people worldwide and most people with asthma have low expectations of what can be achieved by asthma management and don’t realise that their condition can be improved,” said Boehringer Ingelheim’s Head of Respiratory Medicine.
Many people get an initial diagnosis and treatment but never go back to the doctors for a check-up. However symptoms change and science moves forward and it is important to go back to your doctor regularly especially if symptoms lessen or worsen. New drugs, new treatment methods, breathing techniques and supplemental oxygen among other things could be available to you to help to improve your quality of life, reduce the frequency of exacerbations and lessen symptoms. Sleep disturbances could be due to sleep apnoea which could be eased with supplemental oxygen and a slight change to your treatment could greatly improve your oxygen levels, sleep and breathing which would greatly improve your productivity at work and at home.
References: http://lungdiseasenews.com
Injected biosensors could measure your oxygen levels
A company in California has invented biosensors that can be injected into the body and not be rejected by the body's immune system. They could well replace traditional clinical laboratory testing and make our bodies continually accessible 24/7 so that we know exactly whats going on in our bodies and improve our health. The capability for these new biosensors to provide long-term, continuous streams of live data about the levels of various molecules in our body could completely alter the relationship we have with our bodies as well as transforming the healthcare system.
We rarely get the chance to see whats happening inside our body unless we see an x-ray or have specific tests done; we rely on our doctors to take some blood or perform other one-ff tests in order to get a single snap shot of whats going on and interpreting it for us.
If we could see the data for ourselves continuously in real time, then we can make timely choices to prevent symptoms getting worse and have a continuous conversation with our own bodies to keep it within healthy parameters.
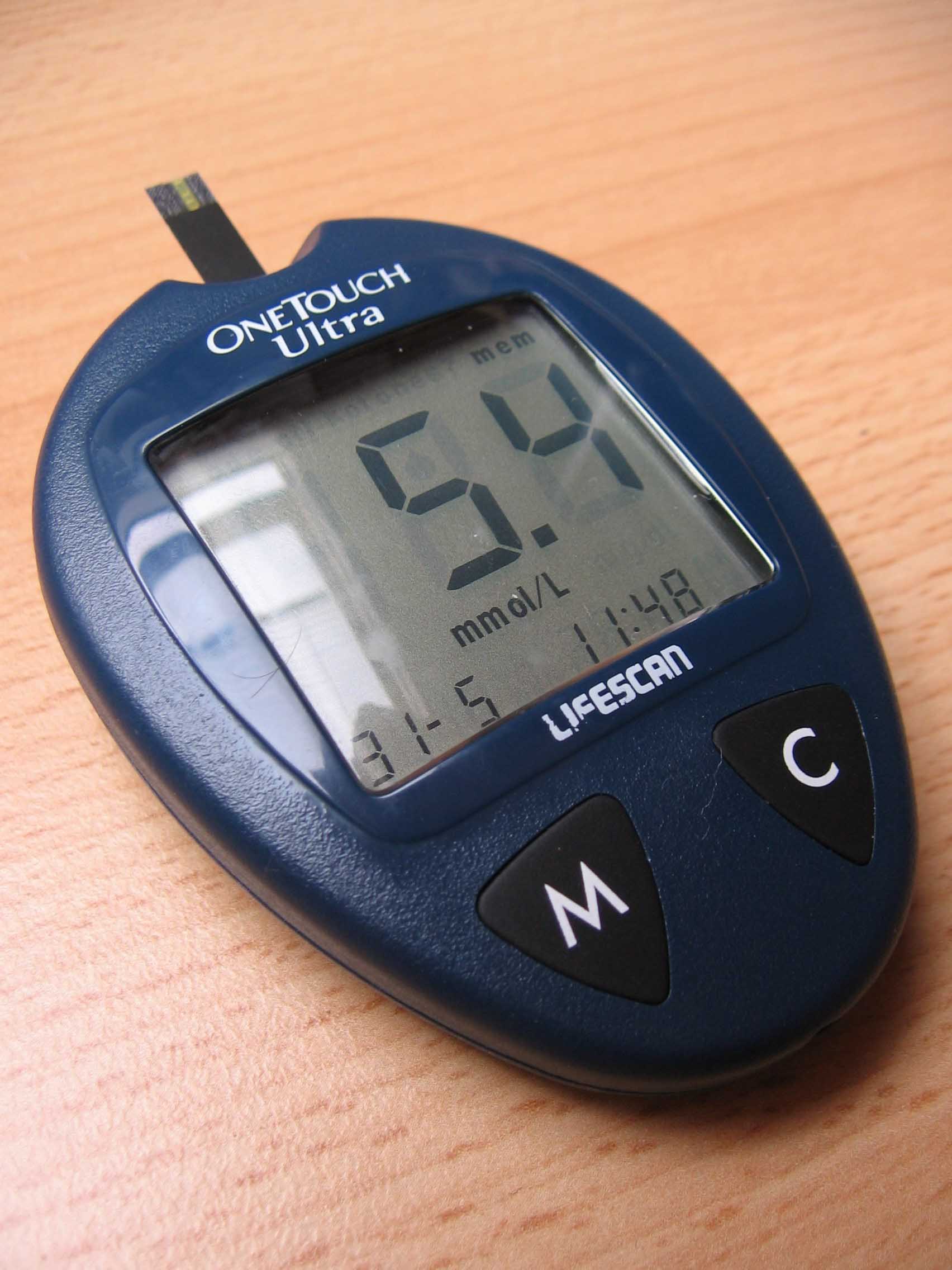
These new biosensors will have uses not only for healthy individuals wishing to remain so and monitor their health and fitness but also could be used in the management of chronic diseases such as diabetes and COPD.
"Our tissue-integrated biosensor technology meets three key criteria for continuous monitoring: First, the data needs to be clinical-grade so that you and your healthcare provider can make medical decisions about your health and wellbeing. Second, the user experience needs to be seamless so adoption can fit into any workflow environment. And finally, the technology needs to be accessible at a reasonable cost in a form function that's easy to use," explained Dr Hwang.
The biggest hurdle of biosensor development has been how to overcome the effects of the foreign body response and to stop the body from rejecting what it thinks are foreign objects. The biosensors are placed under the skin with a specially designed injector. Each biosensor is a flexible fibre of 3-5mm long and 500 microns in diameter. Rather than being isolated from the body these sensors are fully integrated into the tissue of the body. There are no metal devices or electronics involved and therefore overcomes the effect of the foreign body response.
Each biosensor is comprised of a bio-engineered 'smart hydrogel' which is similar to contact lens material which forms a porous, tissue-integrating scaffold that also induces blood vessel growth and cell growth in the surrounding tissue. The smart gel is linked to a florescent light-emitting molecule that continuously signals the presence of a body chemical like oxygen or glucose.
Adhered to the skin's surface or held by hand, a separate optical reader is used to read the fluorescent signal from the embedded biosensor. The reader sends excitation signals through the skin to the biosensor, which then emits light proportional to the concentration of molecules being tracked. The data can be relayed to a smart phone for an encrypted personal record and historical tracking.
Their oxygen sensing system that the company has developed is a single biomarker sensor designed to measure dissolved oxygen in the tissue. It is the only long-term monitoring technology that guides therapeutic action and measures tissue oxygen levels during the treatment and healing process for peripheral artery disease (PAD). It will be available in Europe this year to be used by vascular surgeons and wound-healing specialists. Other respiratory disease patients can also benefit from using this technology such as those who suffer with COPD. They can continuously measure their oxygen levels using real time data in order to be able to adapt and alter medications and supplemental oxygen flow rates in order to prevent exacerbations and hospital admissions. It would help respiratory disease patients to continuously monitor their condition and provide real data for their healthcare provider to monitor and aid in their long-term treatment. It could help prevent exacerbations and help to prolong quality of life and increase survival rates.
In the future we would be able to monitor practically every biomarker in our body and would not need blood tests and some other clinical monitoring tests at hospital to be performed and would reduce the burden upon on the healthcare system. Results could be sent wirelessly to the doctor who could monitor from afar and would change the way medicine is practiced and put the responsibility and control into the hands of the patient.
References: http://www.prnewswire.com
Man's best friend could help with your mobility 24/7
For many people with a lung disease like COPD it can become so restrictive and isolating. Many people get to a stage in their condition where they require oxygen 24/7, which means they are linked to an oxygen canister via tubing permanently, greatly restricting their mobility. It can result in people not wanting to go outside or exercise due to having to deal with the hassle of tubing and concentrators and feeling conspicuous. It is especially difficult for children that have respiratory problems who would normally want to run around and play games.

A child in America has a rare lung disease and she has a specially-trained dog who has been with her since she was little. He carries her oxygen concentrator around and always ensures he doesn't tangle up the tubing and stays within a certain proximity to her. This has meant that not only does the child have a long-term companion to help prevent the feeling of being alone caused by long-term illness, but also allows the child to go out and about, play, exercise and go to school more easily which benefits their health and social development.
This idea of an 'oxygen dog' could be rolled out to people of all ages who require assistance, especially those who are elderly, alone and finding it difficult to cope and get out and about due to their need for 24/7 oxygen. A smaller dog could only carry a portable concentrator however a larger dog would be able to carry a small oxygen tank.
The benefits of having the dog as a puppy when the child is also young is that they can grow and develop together. Different lung diseases at different stages will affect the individual differently so having the dog training at a young age with the patient means that the dog can learn how to deal with different situations and develop with the owner and know how to assist them better and predict movement based on behaviour patterns.
Having a dog is not cheap however and is by no means about to become readily available via the NHS, however it is an avenue that some people may be able to afford or raise funds for as a way to help them enjoy a better quality of life.
References: http://www.stuff.co.nz
Vikings and worms provide clues to the cause of COPD
Revealing Viking Genetics and COPD
Scientists have found evidence that the Vikings may have carried a genetic defect that causes Chronic Obstructive Pulmonary Disease (COPD). According to archaeological digs in Denmark, Viking communities experienced significant worm infestations, which had an impact on their genetic evolution. Although useful in the past, this adaptation is currently associated with a higher risk of COPD.
COPD and the Viking Legacy
The condition known as COPD, which impacts around 5% of the world's population, is greatly impacted by a hereditary alpha-1-antitrypsin (A1AT) deficiency. Due to the evolution of this genetic feature over 2,000 years ago in Viking tribes, it is especially common in Scandinavia.
The protein A1AT shields the liver and lungs, among other important organs, from the protease enzyme. If not controlled, these enzymes—which are made by parasitic worms and the immune system—can seriously harm tissue. COPD is caused by these proteases dissolving lung tissue due to an A1AT deficiency.
Historical Appropriation and Modern Day Consequences
According to Professor Richard Pleass, the Viking diet, which was frequently tainted with parasites, caused their bodies to change. Originally, the aberrant versions of A1AT served as a defence against these parasites, but they now raise the risk of COPD. These variants attach to Immunoglobulin E (IgE), an antibody that worm proteases cannot break down, protecting the Vikings' critical organs.
"In ancient times, these deviant forms of A1AT were crucial for survival against parasitic infections," according to Professor Pleass. "However, with the advent of modern medicine and the eradication of many parasitic diseases, these genetic traits have become a liability, contributing to the development of COPD."
Genetics Today
This finding clarifies why A1AT deficiency still exists in some populations. It implies that if you are of Viking descent, you may be genetically predisposed to COPD, particularly if you smoke or live longer than the Vikings did.
A1AT deficiency's evolutionary history demonstrates how a genetic adaptation that was advantageous in one era can turn out to be harmful in another. This historical viewpoint emphasises the need of knowing our genetic ancestry and offers insightful information about the genetic components of COPD.
The ways that ancient adaptations still affect our health today become more evident as we learn more about our genetic heritage. Knowing the Viking roots of A1AT deficiency sheds light on COPD and emphasises the value of genetic research in the fight against contemporary illnesses.
References
A machine that can help to repair lungs to make them transplant viable
A machine has been developed that can recondition a set of lungs outside of the body in order for them to improve and make them healthier ready for transplant into a recipient. The machine is known as 'the box' and it ventilates lungs after their removal from the donor. It also infuses them with a mix of fluid, drugs and steroids which allows the lungs to dry out and get them into a better shape before being transplanted.
"It allows the lungs to stay alive... and allows us as providers to assess the function of the organ in a unique, well-controlled environment," said Dr. Varun Puri.
The machine is made up of a ventilator to help simulate breathing and a bypass machine to perfuse the lungs with drugs and fluid In order to improve their function and generally helps to mimic the body with one major helpful difference. The lungs normally undergo a lot of stress in the body constantly exchanging gases with every breath, however in this box that stress factor is removed and gives the lungs a chance to heal.
This machine will hopefully help to improve lung transplant statistics and aid in improving the long-term survival rates of those that suffer from respiratory diseases like COPD. Currently fewer than 20% of donor lungs are considered suitable for transplant and 25% of candidates dies whilst waiting for a transplant. Even the survival rate post-transplant is 50% to survive 5 years. This device could aid in increasing the donor pool as the machine can take lungs that were previously deemed as unsuitable and give them a chance to heal and improve, making them then viable lungs for transplantation. With more lungs available for transplant fewer patients will die waiting and if the lungs are healthier when transplanted then hopefully the survival rates for lung transplants will also improve with further research.
“I am sure in the future we will be able to do things like gene therapy to the lungs in a controlled environment or utilizing specific anti-inflammatory agents to prevent short term and long term rejection of organs.” said Dr. Varun Puri.
Michele Coleman, 63, credits 'the box' with saving her life. A former smoker, she was diagnosed with chronic obstructive pulmonary disease and doctors asked if she would participate in a clinical trial.
"You don't want to, but you kind of lose hope because when you are sick like that you know how fast you are going downhill," Coleman said. "It's scary, but anything that they could give me was going to be better than I had, and actually I figured I wouldn't make it to the end of the year," she said. The transplant for her was a huge success and she is still doing well with her 'reconditioned' lungs.
There is also hope of being able to do the same with other organs to improve transplantation survival rates across the board. Hopefully 'the box' brings a little light to those with severe respiratory diseases where their lungs are failing them.
References: http://www.foxnews.com and http://www.trunews.com