A safe and happy flight with portable oxygen
Just because you need to travel with medical oxygen, this need not restrict the opportunities to travel overseas it just takes a little bit more planning. Flying with a Disability offers you the following advice to ensure a safe, happy flight.

Travellers who require oxygen for medical use are, unfortunately, subject to a charge per bottle. This rate varies between airline, and can be quite expensive. You will need to contact the airline at least 48hrs prior to flying to advise the flow rate, and to get full medical clearance, though this tends to be minor technicality.
Charges for portable medical oxygen can vary greatly, usually between £30 and £100 ($50 - $150). It is interesting to note that many airlines charge not per canister, but per leg of your trip. So in a flight which involves two legs, you're going to be charge twice as much a direct flight, despite the fact that you may be covering the same distance in the same length of time.
Economically, therefore, it can work out a lot cheaper if you can organise a direct flight, though this may not always be possible.
If you need help with planning your trip use specialised medical oxygen companies who can help answer all your queries and make your journey stress-free and a safe landing.
There is also some planning whilst safely on the ground with back up services available for portable oxygen concentrators whilst travelling overseas so you can ensure to have a great holiday with medical oxygen.
This should be a worldwide standard...
A top doctor says the roll out of oxygen alert medical bracelets to patients with known Type 2 respiratory failure will help save lives.
Dr Rose Sharkey, Respiratory Consultant, at the Western Health and Social Care Trust, said the easily recognisable purple oxygen alert bracelets will ensure rapid identification of a patient and ensure that ambulance staff transferring a patient to hospital, and doctors are immediately made aware of a patients oxygen therapy needs.
She said: “We have been working closely with our colleagues in the Ambulance Service to ensure Paramedics firstly check if a patient is wearing one of our purple bracelets.
“If so, then can then check the patient’s oxygen alert card which will tell them the correct amount of oxygen therapy to give a patient during an exacerbation of COPD, as they are transferred to hospital. The delivery of excess oxygen to this group of patients can be detrimental.
“The medical bracelets and oxygen alert cards will be distributed to patients attending respiratory clinics and through our Community Respiratory Services.”
Dr Nigel Ruddell, Assistant Medical Director, Northern Ireland Ambulance Service said: “Good emergency care benefits greatly from teamwork, and anything which allows us to work collaboratively with our hospital colleagues to ensure a patient receives optimal care is to be welcomed. We have already seen the benefits of this alert system working elsewhere and are keen to roll it out on a regional basis to make sure that patients across Northern Ireland with complicated conditions can receive tailored treatment from the ambulance service that will mesh seamlessly with their ongoing care.”
COPD: The chronic misery of breathing
Almost always caused by tobacco smoking, chronic obstructive pulmonary disease kills so many people per year. Treatments can’t reverse the symptoms but can halt deterioration.

Some patients say they live with a constant feeling that they are breathing underwater, as if they were always drowning; others describe their breathlessness (even at rest), frequent coughing and never being able to exhale all the stale air in their lungs.
It is chronic obstructive pulmonary disease (COPD), which used to be known as emphysema and chronic bronchitis, but these are only the symptoms and description of changes in the lungs. Emphysema was identified as early as the late 17th century.
In the majority of cases, you yourself have to smoke to get COPD; much less often, victims are non-smokers exposed passively to another’s smoke.
Tobacco is almost the sole cause of COPD in the developed world; a much less common cause is intense and prolonged occupational exposure to workplace dusts, chemicals and fumes; in the Third World, the chronic disease can also result from indoor air pollution in the form of poorly ventilated cooking fires, often fueled by coal or biomass fuels such as wood and animal dung (making women the more common victims).
Of those who smoke, about a fifth will get COPD, but among those who have puffed away for decades, about half will develop it, and the disease will kill many of them. In many developed countries such as the US and the UK, between 80 percent to 95% of COPD patients are either current smokers or previously smoked. There is no cure, but kicking the dirty habit can slow the progression and maybe even improve the situation a bit but can’t cure it; there are medications that can also ease the symptoms, thus early detection is important.
Respiratory rehabilitation and surgery to remove non-functioning lung tissue can also help. Lung transplants can eliminate the problem, but only a few donor organs are available.
Most of the sufferers are over the age of 55, and a majority are male, but due to their smoking habits, women are quickly catching up. By 2020, it is expected that COPD will be the third most common cause of death in the world and the fifth in engendering disability. This trend is ironic, as the prevalence of heart disease, which is also related to smoking, is decreasing. It takes years of exposure to tobacco to produced COPD.
The airways and air sacs are elastic, so when you inhale, each air sac fills up with air like a little balloon.
When you exhale, these sacs deflate and the air exits. But in COPD, less air flows out because the airways and air sacs lose their elastic quality; the walls between many of the air sacs are destroyed; the airway walls become thick and inflamed; and the airways are clogged with mucus.
ALL COPD patients have both chronic bronchitis and emphysema; some have more of one than the other. The first involves a persistent cough, significant amounts of mucus, fatigue, shortness of breath, chest discomfort.
Many patients require oxygen therapy at least 16 hours – and sometimes 24 hours – a day. Most patients have oxygen concentrators (machines that extract oxygen from air) at home.
This does not cure but can help COPD sufferers every day when it comes to breathing to help make it less of a misery.
Fraunhofer develops smartwatch-based assistance and home-health monitoring systems
As our life spans increase, more services and care will be needed for the elderly, especially those who live independently. Technology clearly has an increasing role to play in improving home care and health monitoring. The latest developments from German research group Fraunhofer are interesting to cite.
Wearable home care assistance system
In collaboration with the German Ministry for Education and Research, the Fraunhofer Institute for Photonic Microsystems has created a wearable technology that resembles a smart watch.
- It can be customised to meet the specific needs of an elderly person and is accessed by authorised personnel and carers through an online portal.
- According to Fraunhofer, the concept system offers support services including reminding users to take their prescription or helping them plan their travels to and from the doctor.
- Emergency services can be easily called because it has phone and Wi-Fi access, as well as the ability to directly contact support professionals.
- The large interface (though not quite the largest smartwatch design we've seen) contains a few basic symbols for simple operation and is programmed in advance according to the person’s needs.
Home health monitoring platform
- The Fraunhofer Institute for Applied Information Technology has created a health monitoring system that employs blood sample equipment and tiny, non-invasive sensors to deliver immediate health analysis that can be sent to a physician over the internet.
- Fraunhofer claims that the system, which is centred around a unit housing the software and analytical tools, may monitor parameters such as blood pressure, glucose, lactate, or cholesterol level using wireless sensors. One possible way to use this system is to implant a Bluetooth module in the patient's ear.
- Additionally, the device is capable of analysing blood samples obtained through a finger prick, identifying markers using a fluorescence sensor, and transmitting this data to a physician for review via a mobile app.
According to Professor Harald Mathis of the Fraunhofer Institute for Applied Information Technology (FIT), "miniaturised sensors in the home unit, which can detect traces of the markers down to the nano level, analyse the blood sample."
Sources:
Fraunhofer Institute for Photonic Microsystems
Fraunhofer Institute for Applied Information Technology
Your phone could save your life - one day...
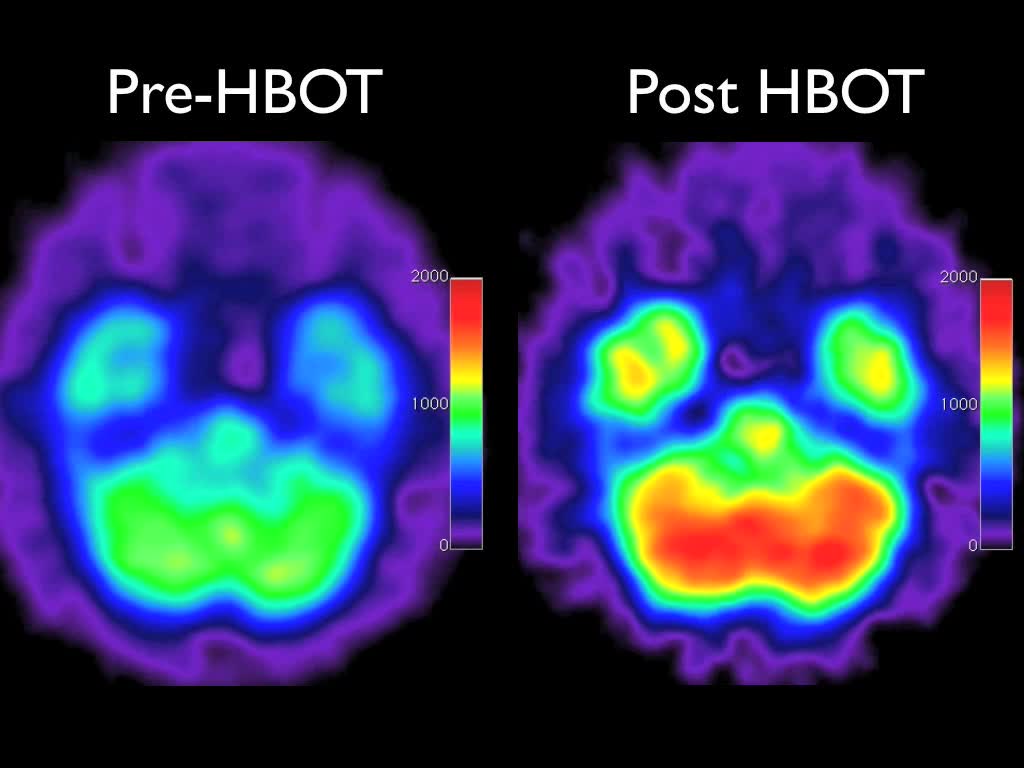
Disease can be treated using pressurized air
Injection For Patients Who Cannot Breathe
An injection that delivers oxygen directly into the bloodstream for patients who cannot breathe has been invented by scientists at Boston Children's Hospital, according a report published in Science Translational Medicine. The authors explained that when patients suffer from an obstructed airway or acute lung failure, they urgently need oxygen to reach their blood, otherwise they have brain injury or suffer from cardiac arrest.
The researchers designed an injection filled with tiny, gas-filled microparticles that can be administered directly into the bloodstream, supplying it with much-needed oxygen.
The microparticles are made of a single layer of fatty molecules that surround a miniscule pocket of oxygen - they are placed in a liquid solution and injected into the patients.
John Kheir and team say that patients who are injected with this solution, may regain near-normal blood oxygen levels within seconds.
In animal experiments, the authors reported that they could beep the animals alive without breathing for 15 minutes, drastically reducing the incidence of organ injury and cardiac arrest (the heart stops completely).
The oxygen injection may buy the patient valuable time John Kheir explained that the microparticle solutions are easy to carry around, and could conveniently be utilized to keep people who cannot breathe alive, giving emergency personnel more time to get patients to a safe place where more sophisticated life-saving procedures can be carried out.
The authors say the microparticle solution injections could not be used for more than fifteen to thirty minutes, because they contain fluid that would overload the blood if used for any longer.
These are not blood substitutes, Kheir stressed. Blood substitutes carry oxygen, but are of limited use when the lungs are not working and cannot oxygenate them. These microparticles are specifically designed for people who cannot breathe.
After caring for a young girl who had severe pneumonia in 2006 and suffered severe brain injury because of extremely low blood-oxygen levels, Kheir starting looking into the idea of injectable oxygen.
The little girl died before the medical team could get her on a heart-lung machine.
It was several years before the team managed to get the microparticles safe for injection. Kheir said "The effort was truly multidisciplinary. It took chemical engineers, particle scientists and medical doctors to get the mix just right."
They used a sonicator - a device which emits high-intensity sound waves to mix lipids and oxygen together. Oxygen gas gets trapped inside tiny particles, about two to four micrometers in size - too small to see with the naked eye. They found that a solution in which 70% of the volume consisted of oxygen was just right for human blood.
In previous studies in the early 1900s, scientists attempted to oxygenate blood with intravenous oxygen, but they failed. Sometimes they caused fatal gas embolisms.
reference: Copyright: Medical News Today
Cluster headaches explained
It was discovered more than a century ago that cluster headaches (CH) are different from migraines. The intense, unilateral pain that this illness creates around the eye has earned it the name "suicide headache" because of how severe it is.
Important Information About Cluster Headaches
1. 1-4 patients per general practitioner in the UK; estimated to be between 34,000 and 150,000 and 3–4 times more common in men
2. Eye, temple, or forehead pain that is quite intense, congestion in the nose, swelling in the eyelids and perspiration of the face
3. The precise cause is unknown, but there may be a genetic component (1 in 20 have a family history)
4. Treatments, both acute and preventative, are advised. Home oxygen therapy up to five times a day for 15 minutes, at 100% oxygen
Treatment with Oxygen for Cluster Headaches 80% of the time, safe and efficient. Used especially for attacks at night and generally regarded as the most successful course of treatment
Alternative Medical Interventions such as home oxygen therapy is still the best option for treating cluster headaches, even though some patients find relief with other therapies like acupuncture.
Our speciality at OxygenWorldwide is offering oxygen treatments for a range of illnesses, including cluster headaches. Our staff can help you set up a portable oxygen supply for travel.
Living without breathing is now possible!
This may seem like something out of a science fiction movie: researchers have designed microparticles that can be injected directly into the bloodstream to quickly oxygenate your body, even if you can't breathe anymore. It's one of the best medical breakthroughs in recent years, and one that could save millions of lives every year.
The invention, developed by a team at Boston Children's Hospital, will allow medical teams to keep patients alive and well for 15 to 30 minutes despite major respiratory failure. This is enough time for doctors and emergency personnel to act without risking a heart attack or permanent brain injuries in the patient.
The solution has already been successfully tested on animals under critical lung failure. When the doctors injected this liquid into the patient's veins, it restored oxygen in their blood to near-normal levels, granting them those precious additional minutes of life.
Particles of fat and oxygen
The particles are composed of oxygen gas pocketed in a layer of lipids, a natural molecule that usually stores energy or serves as a component to cell membranes. Lipids can be waxes, some vitamins, monoglycerides, diglycerides, triglycerides, phospholipids, or—as in this case—fats.
These fatty oxygen particles are about two to four micrometers in size. They are suspended in a liquid solution that can be easily carried and used by paramedics, emergency crews and intensive care personnel. This seemingly magic elixir carries "three to four times the oxygen content of our own red blood cells."
Similar solutions have failed in the past because they caused gas embolism, rather than oxygenating the cells. According to John Kheir, MD at the Department of Cardiology at Boston Children's Hospital, they solved the problem by using deformable particles, rather than bubbles:
We have engineered around this problem by packaging the gas into small, deformable particles. They dramatically increase the surface area for gas exchange and are able to squeeze through capillaries where free gas would get stuck.
Kheir had the idea of an injected oxygen solution started after he had to treat a little girl in 2006. Because of a lung hemorrhage caused by pneumonia, the girl sustained severe brain injuries which, ultimately, lead to her death before the medical team could place her in a heart-lung machine.
Soon after, Kheir assembled a team of chemical engineers, particle scientists, and medical doctors to work on this idea, which had promising results from the very beginning:
Some of the most convincing experiments were the early ones. We drew each other's blood, mixed it in a test tube with the microparticles, and watched blue blood turn immediately red, right before our eyes.
It sounds like magic, but it was just the start of what, after years of investigation, became this real life-giving liquid in a bottle.
This is what the future is about. And it's a beautiful one indeed, one that is arriving earlier than we ever could have expected. I wonder if this would find its way to other uses. I can see it as an emergency injection in a spaceship, for example. But what about getting a shot for diving? [ScienceDaily]
Image by Filip Fluxa/Shutterstock