Iron deficiency can worsen COPD symptons
Scientists believe that those who suffer from lung disease may suffer more severe symptoms due to a shortage of iron, which could be easily rectified with regular intravenous iron injections.

Iron deficiency is more common in patients with COPD than in those without the lung condition, according to the results of a study published in the BMJ. Its been found that one in five COPD patients has iron deficiency and these patients also suffered from lower oxygen levels, more frequent flare-ups and increased shortness of breath and coughing. Iron-deficiency is traditionally associated automatically with anaemia but iron is essential for many other processes within the body.
“We were really quite surprised how big the differences in oxygen levels were between patients with low iron and those with normal iron levels. The amount of oxygen in the blood is a strong predictor of life expectancy in COPD, so these findings are potentially very significant for patients,” says Professor Peter Robbins from the University of Oxford who led the work.
Levels of C-Reactive Protein are significantly higher in iron-deficient COPD patients, which means inflammation. The inflammation is driving the iron deficiency and the idea that inflammation causes iron deficiency is important. It suggests that other conditions may also result in iron-deficiency caused by inflammation and that other conditions could be treated with iron to help reduce the secondary symptoms caused by a lack of iron. Intravenous iron therapy has been shown to be beneficial in other chronic disease and should be explored as a potential new treatment for COPD patients.
Giving up smoking is the most important thing to do if you have COPD but many patients are still left with troubling symptoms that interfere with their daily lives and can lead to hospital admission. The current treatments target the airways which helps some symptoms but doesn't improve the patient's exercise ability and quality of life as much. Iron deficiency seems to act in a variety of ways to worsen the impact of COPD so treating patients with iron can help improve patient's quality of life, exercise abilities and general symptoms and reduce exacerbations.
There is the counter argument that iron injections would not resolve the problem as the patients usually are not short of iron in their food intake, it is just how the body utilises the iron when suffering from bouts of inflammation that causes the anaemia. Increasing the levels of dietary iron intake will therefore not resolve the issue however perhaps taking iron in the form of a supplemental multivitamin may help.
More research is needed into how best to correct the iron-deficiency and improve the lives of COPD patients.
References: http://www.telegraph.co.uk and http://www.pharmaceutical-journal.com
10 Christmas gift ideas for someone with COPD
Obviously friends or family with COPD do not just want presents all about their illness but if they have been newly diagnosed or need items replacing then you might be able to get them the perfect present. Anything that can help them with their disease will mean that you've helped to improve their quality of life all year round.

- Exercise Bike
Nothing is more important to the person who has COPD than exercise. Exercise helps build endurance and muscle strength, ultimately making it easier for your loved one to breathe. An exercise bike helps that person to enjoy exercise within the comfort of home with their oxygen nearby for peace of mind, and they can use it all year round in any weather condition, unlike a normal bike.
- Pulse Oximetry Monitor
An FDA approved pulse oximetry monitor allows the patient to monitor their oxygen levels to ensure that they are getting enough.
- Automatic Blood Pressure Monitor
Many patients suffer from COPD complications and may take a variety of different medications for them. A blood pressure monitor is essential to make sure the medications or the condition are not affecting their health.
- Nebulizer
A nebulizer is important to have as it administers medication directly into the COPD patient's airways to help them to breathe easier. Handy to have one when out and about so that if an attack happens they can try to reduce it and improve their breathing as a short-term tactic until they can get to their oxygen supply.
- Knitted Beret, Scarf and Gloves
Keeping warm is so very important for someone with COPD as cold air can trigger an attack and they will help to prevent them from catching any bugs during the winter.
- Nebulizer Carry Bag
This will allow them to take their nebulizer out and about with them more easily and help to encourage them to keep themselves active. It could be used to carry other small pieces of equipment too.
7.Extended Oxygen Tubing
If they feel slightly shackled to their oxygen tank then getting them some extended tubing will allow them more freedom of movement in their home to be able to do more homely activities and keep them more active at home.
- COPD for Dummies Book
A great beginner's guide for someone newly diagnosed or their partner or carer with lots of tips and advice on how best to cope with COPD. Also if they are smokers then perhaps self-help books on stopping smoking could also be beneficial.
- Portable Concentrator
If their local provider cant provide them with one then you can buy one privately. A portable concentrator is a hugely beneficial piece of equipment as it allows the patient to leave their home free from the shackles of their tank and use oxygen easily outside. It gives the patient a huge new lease of life and allows them to exercise, go shopping, see friends etc. without having to take their oxygen tank and supporting equipment with them.
- Accessories
There are lots of accessories available to help improve the home for patients who use oxygen. Sometimes local providers have limited choice and availability of these neat gadgets but private companies have a vast choice of those small things that can make a huge difference.
References: www.copd.about.com
Lung freezing may be a new treatment for COPD
Bronchitis is one of the diseases that falls under the COPD umbrella. It is where the main airways become inflamed and irritated leading to shortness of breath, mucus build-up and severe coughing. The new treatment being tested on patients with chronic bronchitis targets the thickened airway tissue by freezing it via a technique known as cryotherapy.
The theory behind it is that the cycle of freezing and thawing destroys the damaged tissue in the lungs allowing healthy cells to develop in its place and helps to repair the lungs and improve breathing. This has already been used to successfully treat oesophageal cancer.
A catheter is inserted into the airway and navigated to where the airways are thickened via an MRI scan and then liquid nitrogen at -200C is sprayed onto that section. The section of lung tissue is then allowed to naturally thaw for a few minutes and then the area is repeatedly blasted until the target tissue has been destroyed. The flash-freeze and slow thaw of the tissue has been shown to destroy the targeted cells but does not affect the collagen, which provides the scaffold for healthy tissue to regrow into.
This is currently being trialled in several British Hospitals and appears to be successful. The treatment can be adapted according top the patients needs and the number of treatments will depend upon the severity of their condition and how much tissue needs to be frozen. Hopefully these trials are the start of a journey towards a new successful treatment for COPD.
The medical potential is vast as it could mean that damaged tissue anywhere in the body could be treated by cryotherapy in the same way and allow new tissue growth to come through, thereby allowing aided self-healing of a huge number of conditions.
References: www.dailymail.co.uk
SLEEP APNOEA MAY CAUSE ALZHEIMER'S AND SUPPLEMENTAL OXYGEN COULD PREVENT IT
Alzheimer's disease is the most common form of dementia, which is a set of symptoms that include memory loss and problems with thinking, problem-solving and language. It is a physical disease that affects the brain and proteins build up in the brain forming 'plaques' and 'tangles' around the nerves. Connection is then lost between the nerves cells and leads to the death of the nerve cells and loss of brain tissue. Patients with Alzheimers also have a shortage of important chemicals that help to transmit signals around the brain. The disease is progressive and as more of the nerve cells die and brain tissue is lost, the more severe the symptoms.
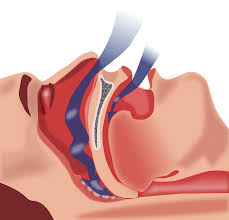
Sleep apnoea is a condition where the walls of the throat relax and narrow during sleep and interrupts normal breathing patterns. During an episode the lack of oxygen triggers your brain to pull you out of your deep sleep so that your airway reopens and you can breathe normally. After falling back into a deep sleep again further episodes can occur even as frequently as every few minutes. Most patients snore loudly and have laboured and noisy breathing and is often interrupted by gasping and snorting. This repeated sleep interruption can make patients feel extremely tired during the day and suffer from reduced mental ability. However unless a partner or family member notices your symptoms whilst you sleep you may not know that you suffer from this condition and many people go undiagnosed.
Recent studies have shown that sleep apnoea may quicken memory decline and bring forward the onset of memory impairment conditions like Alzheimers by 10 years. The development and progression of Alzheimers may also be speeded up by sleep apnoea as well. These studies also revealed however that sleep apnoea patients that were being treated with supplemental oxygen overnight delayed the onset of memory impairment problems by as much as 10 years. Patients with sleep apnoea who were being treated declined at the same rate as volunteers who did not have sleep apnoea showing that being treated by oxygen counteracted the harm being done by the condition. It appears that the frequent drops in oxygen levels during episodes of untreated sleep apnoea have a major impact upon memory impairment and can directly lead to the early development of Alzheimer's and dementia. Also during sleep is when the brain has time to remove harmful waste products, if sleep is disturbed then there is an accumulation of harmful proteins that block nerve cell function. Certain parts of the brain are more sensitive to drops in oxygen levels than others; certain neurons in the hippocampus (where Alzheimer's is thought to start) is especially sensitive to drops in oxygen and sleep apnoea may 'stress' these neurons out.
There are currently no medications that can prevent the progression of mild cognitive impairment to Alzheimer's disease or dementia so treating at-risk patients with CPAP (oxygen treatment for sleep apnoea) is a prevention method that is worth trialling and testing. Previous research has already shown that CPAP treatment and supplemental oxygen at night slows and improves cognitive impairment in patients with Alzheimer's disease and increases brain tissue and now this more recent research backs up these findings. Hopefully soon there will be trials to prove whether supplemental oxygen at night could be the next new treatment for Alzheimer's and dementia patients or even those who are at risk.
References: www.nbcnews.com, www.alzforum.org, www.alzheimers.org.uk and www.nhs.uk
What is PAM?
PAM stands for pulmonary alveolar microlithiasis, which is a rare lung disease. It is where small stones accumulate in the alveolar air sacs in the lungs and therefore makes it increasingly difficult to breathe. The cause has been found to be due to a DNA mutation which results in the loss of a cellular pump which would normally remove excess phosphate from the air sacs. As a result there is a build-up of calcium and phosphate which leads to the formation of microliths or stones. These cause chronic inflammation, lung tissue damage and scarring and respiratory failure and patients require a continuous oxygen supply of a high oxygen concentration in order for patients to be able to get enough oxygen into their bodies to function.
New research has identified biomarkers, which may hold the key to being able to treat this rare and debilitating disease. It seems that the condition causes elevations of certain proteins (cytokines and surfactant) in the blood. By monitoring these levels doctors will be able to follow disease progression and treatment response in patients.
Another finding was that the stones dissolve in EDTA which is used currently as a treatment for heavy metal poisoning. If the lungs can be washed in a solution containing EDTA then the stones could be dissolved and reduce the burden being placed on the air spaces and relieve respiratory symptoms. As long as there are no toxic side-effects then this could become a new therapy for patients with PAM.
As the stones are caused by excess phosphate it has been surmised that a low phosphate diet may be able to prevent the formation of the stones, however a phosphate-restricted diet brings with it other medical problems such as rickets. Another possible idea is to restore the function of the pump in the cells by inserting a phosphate pump gene into the DNA of the cells using viral vectors.
"This study demonstrates how discovering the causes of these rare lung diseases not only can inform us how the lung normally functions, but can also lead us to potential therapeutic interventions for these rare and often lethal lung diseases,” says James Kiley, PhD, Director of the Division of Lung Diseases at NHLBI.
Rare disease research can reveal insights into the fundamental biology of the lung and this study for PAM has revealed a potential role for phosphate in the regulation of surfactant balance in the lung and have attracted the interest of cystic fibrosis scientists who may be able to use the findings to help treat CF.
References: http://healthnews.uc.edu and http://medicalxpress.com
PINEAPPLE JUICE COULD HELP WITH YOUR COUGH
Pineapple juice has been shown to be 5 times more effective than cough syrup. It fights infection, kills bacteria, loosens mucus and suppresses coughs.
 Pineapple juice contains an enzyme called bromelain, which has anti-inflammatory properties and is effective to combat lung inflammation. It is used to treat arthritis and is also used in the treatment of inflammation and swelling in the nose and sinuses. 1 cup also contains half of your daily requirement of Vitamin C intake. Vitamin C is essential because as well as many other uses, it also enables your body to metabolize certain vital enzymes that regulate your metabolism and manage energy. Pineapple juice also contains manganese, which is a mineral that helps form healthy connective tissue and bones. It also works to absorb more calcium, metabolize carbohydrates and fats and increases regular nerve function. Pineapple juice helps to soothe sore throats and helps to loosen and expel mucus from your lungs more easily.
Pineapple juice contains an enzyme called bromelain, which has anti-inflammatory properties and is effective to combat lung inflammation. It is used to treat arthritis and is also used in the treatment of inflammation and swelling in the nose and sinuses. 1 cup also contains half of your daily requirement of Vitamin C intake. Vitamin C is essential because as well as many other uses, it also enables your body to metabolize certain vital enzymes that regulate your metabolism and manage energy. Pineapple juice also contains manganese, which is a mineral that helps form healthy connective tissue and bones. It also works to absorb more calcium, metabolize carbohydrates and fats and increases regular nerve function. Pineapple juice helps to soothe sore throats and helps to loosen and expel mucus from your lungs more easily.
The study also indicates that the bromelain naturally present in pineapple may provide similar effects if the cough you suffer from is due to asthma. Pineapple juice has also been used to treat other respiratory ailments such as bronchitis, hay fever, asthma and pneumonia. It’s even being tested as a possible treatment for cancer and HIV.
Drinking pineapple juice instead of cough syrup is less expensive and has no toxic chemicals. Also a study also showed that when using pineapple juice patients recovered nearly 5 times faster from their ailments and exhibited a decrease in other symptoms related to coughing such as hacking.
If you suffer from persistent coughing from respiratory conditions such as COPD and asthma then by drinking pineapple juice not only does it soothe related ailments from persistent coughing but it suppresses the cough and helps to loosen mucus build-up and also aids in combating lung inflammation. This in itself can hugely improve your quality of life, help you to breathe better and help to reduce your symptoms and improve your condition. The naturally-occuring components also have other health benefits to aid in your overall health.
References: http://preventdisease.com and http://www.survivalmagazine.org
Tips to help you get through the flu season
The Flu season is upon us and is generally considered to be the worst time of year for COPD patients and others that suffer from respiratory conditions. Because COPD often affects the immune system, as well as the ability to recover from common illnesses, you need to be vigilant to try and protect yourself from catching colds and the flu. Sometimes its difficult to tell whether you've just got a cold or the flu, but as both can exacerbate COPD it's important to be able to distinguish between the two.
 A cold usually begins with a sore throat followed by clear, watery nasal drainage, sneezing, fatigue and sometimes a slight fever. A mild cough is a common cold symptom and usually lasts into the second week of the cold. If you are coughing up dark mucus then you may have a bacterial infection and should see your doctor. A more severe fever or other symptoms would indicate that it is more likely to be the flu. With the flu your symptoms are more severe and you can feel very weak and fatigued for up to three weeks.
A cold usually begins with a sore throat followed by clear, watery nasal drainage, sneezing, fatigue and sometimes a slight fever. A mild cough is a common cold symptom and usually lasts into the second week of the cold. If you are coughing up dark mucus then you may have a bacterial infection and should see your doctor. A more severe fever or other symptoms would indicate that it is more likely to be the flu. With the flu your symptoms are more severe and you can feel very weak and fatigued for up to three weeks.
Each year the typical adult can expect to contract a cold twice and 50% risk of catching the flu. When you have conditions such as COPD your immune system is compromised and the damage to your lungs and airways and reduce the normal effect that the body has at naturally protecting itself from germs. There are lots of tips on how to prevent yourself from getting ill, to avoid exacerbations and to cut short the duration and reduce symptoms of your illness.
Eat yogurt for breakfast
The same live cultures that help ease digestive distress can help stave off a cold. Scientists found that people who consumed probiotics had 12 percent fewer upper respiratory infections. Research also showed that the group that took a probiotic supplement with Lactobacillus rhamnosus recovered two days earlier and had symptoms that were 34 percent less severe.
Open a window
Spending the day in a stuffy room with anyone who's under the weather raises your risk of catching a bug. Letting a little fresh air circulate keeps airborne viral particles on the move, making them harder to pick up.
Turn away from sneezers
Moving out of firing range is crucial as germs carried in sneeze particles can travel 20 feet.
Stop touching your lips
Not touching your face greatly reduces your odds of getting sick. The average person puts a hand on her mouth or nose more than three times an hour. To break the habit, try sitting on your hands when they're idle.
Get regular sleep
A study found that subjects who slept for fewer than seven hours were nearly three times as susceptible to colds as people who slept for at least eight hours.
Flush out your nose
Throughout cold season, add this to your night-time routine: Rinse your nose using an over-the-counter nasal irrigator or saline solution as it will help clear out viral particles you've breathed in during the day before they take root in your system.
Zinc lozenges
Try taking these within 24hrs of the onset of a cold and it will reduce the duration. You can also eat zinc-rich foods. Zinc is a mineral essential to the cells of the immune system and can boost your libido, help wound healing and prevent excessive inflammation.
Keep hydrated
Fluids help to thin out the mucus that your body makes when you're sick and makes it easier to clear out of your system.
Try elderberry extract
A syrup made from these berries has long been used as a folk remedy for viral infections. The berries' nutrients seem to offer some relief from congestion, aches and pains and can cut short flu symptoms by four days.
Switch on a humidifier
Dry indoor air makes a sore throat and cough even worse. A humidifier helps these symptoms become more bearable by filling the air you breathe with moisture.
Inhale essential oils
Several times a day, add a few drops of thyme or eucalyptus oil to boiling water, then breathe in the aromatic steam. The menthol-like smell should make your airways feel as if they're opening up. It's also thought that antimicrobial particles in these essential oils coat the mucous membrane lining the nasal cavity.
Don't over-exercise
A bit of light exercise such as walking or yoga can make you feel better and boost your circulation but don't overdo it as your body needs to conserve energy to fight off the virus.
Gargle with warm salt water
Salt helps kill pathogens and by coating your throat with a salt solution (1/2 teaspoon of salt in a cup of warm water) will ease inflammation and loosen mucus, which helps flush out germs.
Heat up chicken soup
The steam helps open stuffed-up nasal passages, and the salty broth can soothe a sore throat. Research published found that chicken soup has properties that slow the movement of infection-fighting white blood cells; when they move more slowly, they spend more time in the areas of the body that need them most.
Have a spoonful of honey
Honey is believed to be antimicrobial, and its thick, syrupy consistency coats and soothes an irritated throat.
Prop yourself up
When you lie on your back, mucus collects in your sinus cavities, which can lead to secondary infections or chronic sinusitis. Instead, try resting and sleeping at a 45-degree angle. Sitting up slightly will also help blood flow away from the head reducing inflammation of the sinuses and nose.
General tips this flu season include:
- Washing your hands regularly. Something as simple as a shopping trolley handle, or even a doorknob, can harbour germs. These germs are then entered into our respiratory tract when we touch our face. Washing your hands regularly will reduce the likelihood of catching an illness.
- Avoid people who are sick. Avoid being in crowded places in public where possible, perhaps go shopping in quieter periods. Consider wearing a surgical masks when you are around large groups of people during peak cold and flu seasons.
- Diet is very important in COPD management. Aa person with COPD uses a large amount of calories just to breathe and it is important that you get enough “healthy” calories each day to offset this deficit. You should be eating balanced meals and they should also be smaller and more frequent throughout the day. Large meals can actually cause breathlessness (if you use oxygen, wear it while you eat) and digesting large meals actually consumes a large amount of calories that you need to breathe.
- Get into a regular exercise Doing a little bit each day will improve your health and medical conditions and help to prevent contracting any more illnesses however ensure it is an exercise routine that is safe, comfortable and effective for you. Talk to your doctor for suggested exercise types that would suit you.
References: www.copdfoundation.org and http://edition
Low oxygen levels affect your dna

When cells are functioning normally the DNA structure within them is open in order for molecules to be able to access parts of the genetic code that it contains. This is so that important proteins can be instructed to be made and allow the cell to function.
A new study has found that when a cell is starved of oxygen it results in the DNA strand coiling up and compacting itself into tight clusters. This means that molecules cannot access the DNA strand, the genes cannot be read as easily and the cell's activity is reduced and the cell effectively shuts down resulting in cell death.
This starved state is seen in common diseases like heart attacks, stroke and cancer. However it is also important for those that suffer from any condition that results in low oxygen levels in the body such as COPD, sleep apnoea and asthma. Low levels of oxygen trying to circulate around the body tend to be prioritised to the more important organs and other areas see low/starved oxygen levels. It highlights the importance of monitoring your oxygen levels and ensuring that you use your supplemental oxygen to ensure that you have adequate levels of oxygen in your body.
If low oxygen results in DNA compaction and cell death then it could help to explain why COPD sufferers often experience a combination of various other health conditions and diseases.
When a person suffers a heart attack or stroke, it can cause long-term damage because the restricted blood supply to the heart and brain starves the affected cells of oxygen and nutrients (ischemia). Oxygen starvation (hypoxia) can also result from other disease conditions, such as in cancer tumours. When this happens to cells in the heart, it leads to a heart attack and when it happens in the brain, it leads to a stroke.
Senior author Dr. George Reid explains:
"When you have a stroke, when you have a heart attack, this is likely to be what's happening to your DNA. Now we know that this is what's going on, we can start to look at ways of preventing this compaction of DNA."
If drugs for example can be developed to prevent this DNA contraction then it may prevent long-term damage from strokes and heart attacks as well as a host of other medical conditions that afflict suffers of respiratory diseases.
References: http://www.medicalnewstoday.com and http://www.sciencedaily.com
Breathing is the key to...breathing!
Those that suffer with respiratory conditions such as COPD and Asthma often need supplemental oxygen to aid in delivering more oxygen to the body. However some still find breathing difficult. Struggling to breathe properly may only be noticeable to some when trying to perform strenuous tasks or exercise. Two of the most common problems are over-breathing (hyperventilation) and mouth breathing, which both can have huge health impacts, particularly during exercise.
 You may think that you know how to breathe properly, we all do it every day in order to stay alive however many of us breathe in such a way that it puts our health in jeopardy. If we can breathe correctly then we will be able to ensure that the most efficient amount of oxygen possible is reaching our lungs and reduces any related health problems and improves quality of life for those with respiratory conditions.
You may think that you know how to breathe properly, we all do it every day in order to stay alive however many of us breathe in such a way that it puts our health in jeopardy. If we can breathe correctly then we will be able to ensure that the most efficient amount of oxygen possible is reaching our lungs and reduces any related health problems and improves quality of life for those with respiratory conditions.
HYPERVENTILATION:
Over-Breathing is defined as 'breathing in excess of metabolic requirements of the body at that time' and traits include:
- Mouth breathing
- Frequent sighing
- Taking a large breath prior to talking
- Upper chest moves visibly with each breath
- Regular sniffing
- Erratic breathing
- Noticeable or audible breathing during rest
- Yawning with big breaths
- Nasal congestion
- Sleep apnea
Once the pattern of over-breathing has set in it becomes a chronic condition which will require the person to relearn how to breath correctly to break the habit. Chronic over-breathing can lead to various conditions:
- Heart palpitations and other irregular heart beat conditions
- Cold hands and feet and numbness
- Headaches
- Chest pain
- Dizziness and fainting
- Muscle cramps
- Panic attacks
- Bloating and acid reflux
- Weakness and exhaustion
- Poor memory and concentration
- Sleep disturbances and excess sweating
Over-breathing results in removing too much carbon-dioxide from the body. Carbon-dioxide is seen as just a waste product of breathing however the body does need a small amount as it helps to maintain your blood pH.
Over-breathing results in more air being inhaled but it actually reduces the amount of oxygen being delivered to the body and it can lead to constriction of the arteries.
DYSFUNCTIONAL BREATHING:
Those with Asthma and Sleep apnea tend to breath in up to 3 times as much air as those who breathe normally, which happens due to breathing deeper and more frequently.
This dysfunctional breathing can be caused by:
- Processed foods which form acid
- Overeating
- Stress
- Asthma
- Thinking that it's good practise to take big deep breaths
- Lack of exercise
- Genetic predisposition
- High temperature indoors
- Excessive talking
Stress plays a huge role as many of us suffer this on a frequent basis. If you chronically over-breathe then it does not take much to push your body over the edge, even a minor stressful event can provoke symptoms such as heart problems or a panic attack. It isn't in fact due to the stress factor but to the chronic over-breathing. A traditional solution to panic attacks was to breathe into a paper bag however a more permanent solution is to address the way you breathe. Conventional advice of deep breathing actually worsens the situation and in fact the best way to address stress is to slow down your breathing and to breathe lightly. This reduces the number of breaths per minute and also the amount of air volume being inhaled.
HOW TO BREATHE BETTER:
Ideally your breathing should be light, soft and gentle to the point where the fine hairs in the nostrils remain motionless. Also importantly you should breath through your nose and not your mouth. In fact your nose performs around 30 different functions which are all important linked to your lungs, heart and other organs. Nose breathing is also important as there is nitric oxide in your nose which is carried down to your lungs and it helps to maintain homeostasis in your body and helps to open your airways and blood vessels as well as having antibacterial properties. It also reduces the tendency to take in a bigger breath than is necessary.
The Buteyko Breathing Method:
There is a simple test you can do to measure your levels of carbon dioxide:
- Sit straight without crossing your legs and breathe comfortably and steadily.
- Take a small, silent breath in and out through your nose. After exhaling, pinch your nose to keep air from entering.
- Start counting and hold your breath until you feel the first definite desire to breathe.
- When you feel the first urge to breathe, resume breathing and note the time. The urge to breathe may come in the form of involuntary movements of your breathing muscles, or your tummy may jerk or your throat may contract. This is not a breath holding competition — what you're measuring is how long you can comfortably and naturally hold your breath.
- Your inhalation should be calm and controlled, through your nose. If you feel like you must take a big breath, then you held your breath too long.
The time you just measured is called the 'control pause' or CP, and it reflects the tolerance of your body to carbon dioxide.
- CP 40 to 60 seconds: Indicates a normal, healthy breathing pattern, and excellent physical endurance
- CP 20 to 40 seconds: Indicates mild breathing impairment, moderate tolerance to physical exercise, and potential for health problems in the future (most folks fall into this category)
- CP 10 to 20 seconds: Indicates significant breathing impairment and poor tolerance to physical exercise; nasal breath training and lifestyle modifications are recommended (potential areas are poor diet, overweight, excess stress, excess alcohol, etc.)
- CP under 10 seconds: Serious breathing impairment, very poor exercise tolerance, and chronic health problems.
The shorter your CP then the more breathless you'll get during exercise. If it is less than 20 seconds then never breathe your mouth when exercising and especially if you suffer from asthma. By increasing your CP even by 5 seconds will result in you feeling better and improve your exercise tolerance.
To improve your CP you should follow the following breath hold exercise. However if you suffer from cardiac problems, high blood pressure, panic attacks, are pregnant or have Type 1 Diabetes then ensure you do not hold your breath beyond the first urges to breathe.
Repeat the following exercise several times in succession, waiting about 30 to 60 seconds in between rounds, and do the exercise on a regular basis.
- Sit up straight.
- Take a small breath in through your nose, and a small breath out.
- Pinch your nose with your fingers and hold your breath. Keep your mouth closed.
- Gently nod your head or sway your body until you feel that you cannot hold your breath any longer. (Hold your nose until you feel a strong desire to breathe.)
- When you need to breathe in, let go of your nose, and breathe gently through it, in and out, with your mouth closed.
- Calm your breathing as soon as possible.
By retraining yourself to breathe correctly and more efficiently it can have a hugely noticeable impact upon your breathing, oxygen delivery, health, ability to exercise and overall quality of life.
References: http://articles.mercola.com and http://www.buteykoclinic.com
Facial hair can be dangerous
Millions of people suffer with respiratory problems that require them to utilise home oxygen therapy. A portable device delivers oxygen-rich air via tubing to the nose to aid patients in increasing their oxygen intake.
After a trend was noticed in patients suffering from facial burns, research and studies have been carried out which suggest that men who use home oxygen therapy are at a higher risk of serious facial burns. A major factor involved was the presence of facial hair such as moustaches.
NASA had already investigated the fact that human hair ignites more readily in the presence of higher oxygen concentrations but no-one had previously looked into this within the context of oxygen therapy. To test their theory they used mannequins with nasal tubing and exposed them to a spark. Those mannequins with a moustache ignited whereas those without facial hair did not.
“If you’ve ever tried to start a camp fire, you always start with some dry little twigs and once that starts - and that’s kind of the moustache - then that oxygen tubing lights on fire, it’s like a blow torch shooting up their nose,” said Dr. Andrew Greenlund of the Mayo Clinic in Rochester, Minnesota. Moustaches and other facial hair can act as kindling for nasal oxygen tubes when a spark joins the mix, even if the spark is just a tiny ember that flies at an oxygen tank user from a match, grill or fireworks.
Avoiding a potential spark in the first place is paramount such as to not smoke whilst using oxygen therapy and to stay away from grinding metal and open flames. Being clean-shaven however would prevent facial burns if there was an accidental spark exposure. If your culture and religion allow it then shaving facial hair would be the main preventative measure in eliminating the risk of facial burns. However if a man decides to keep it then using water-based products rather than oil or alcohol-based ones would help to reduce the risk. Also the poly-vinyl tubing is highly flammable and ideas are being researched into changing the material that the tubing is made from so that it doesn't burn as easily.
The burns that can occur from a single spark can be very severe and the burns can also travel beyond the external facial skin and cause damage to the inner nose, mouth and airways, causing swelling and tissue death. The degree of the burn can vary but can be serious enough to result in the patient being put on a ventilator whilst the burns heal. They can result in scarring and worsening of their health. The experience of being burnt can be emotionally stressful too, described by one victim as 'like looking hell in the face.'
The incidence of facial burns have gradually been increasing as more people utilise oxygen therapy and are especially high in the winter, as more men tend to grow beards and moustaches during colder weather. Also the incidence of home fires in general have risen in homes where oxygen therapy is being used and the facial burns can result in a spark from that mini fire on a patient's face catching other things in the home on fire such as clothing and fabrics.
However as long at users are aware, reduce all risk factors and are careful then there is nothing to worry about.
References: www.reuters.com and www.sciencedaily.com













